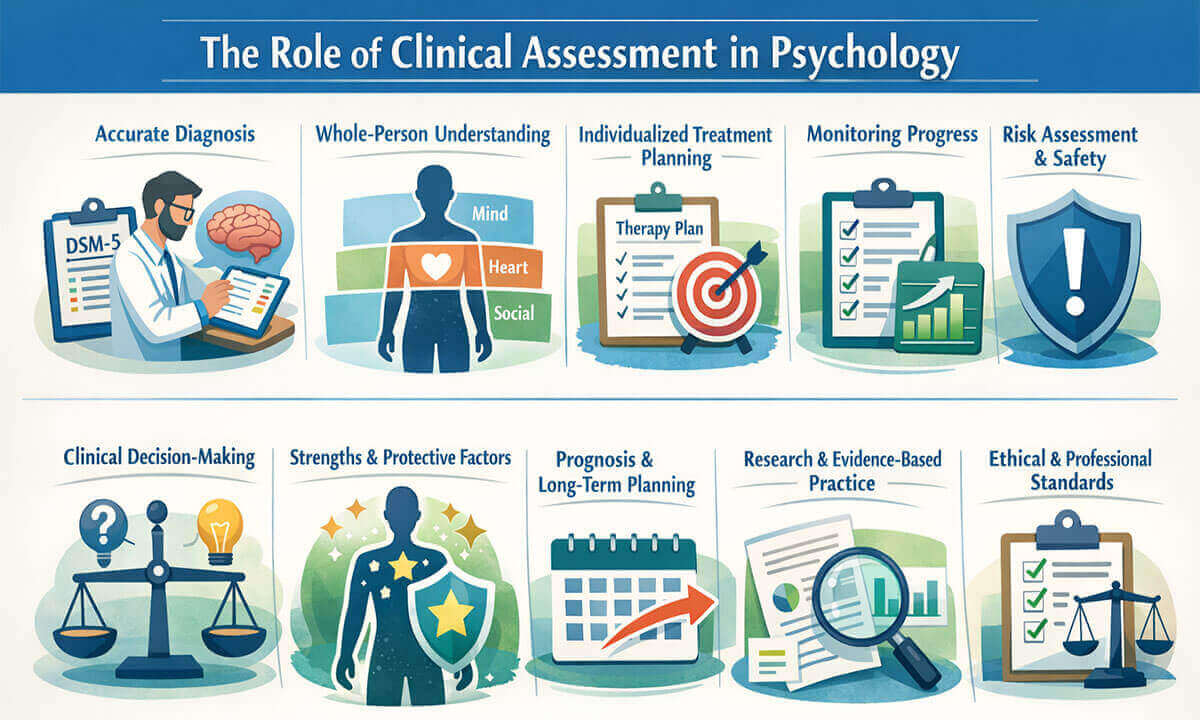
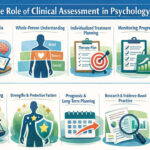
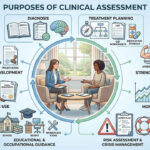
The Role of Clinical Assessment in Psychology:
Clinical assessment is one of the foundational pillars of psychological practice. It serves as the bridge between psychological theory, empirical research, and real-world clinical intervention. Through systematic evaluation of an individual’s thoughts, emotions, behaviors, and functioning, clinical assessment enables psychologists to understand complex psychological difficulties and make informed decisions about diagnosis, treatment, and prognosis. Unlike a single test or interview, clinical assessment is a dynamic, multi-method, and ongoing process that evolves as new information emerges (Groth-Marnat & Wright, 2016). In modern psychology, clinical assessment plays a crucial role not only in diagnosing mental disorders but also in treatment planning, monitoring progress, risk management, and ethical decision-making. In the rest of this article, we will explore the role of clinical assessment in psychology.
1. Facilitating Accurate Psychological Diagnosis: A central role of clinical assessment in psychology is to facilitate accurate and reliable psychological diagnosis. Diagnosis in clinical psychology is not based on intuition or isolated observations; rather, it emerges from a systematic integration of data gathered through multiple assessment methods, including clinical interviews, standardized psychological tests, behavioral observations, and collateral information from family members or other professionals (Groth-Marnat & Wright, 2016).
Clinical assessment helps psychologists determine whether an individual’s symptoms meet the diagnostic criteria specified in classification systems such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) (American Psychiatric Association [APA], 2022). Many psychological disorders share overlapping features (such as sleep disturbance, concentration problems, or emotional dysregulation) making differential diagnosis particularly challenging. For example, symptoms of major depressive disorder may overlap with generalized anxiety disorder or post-traumatic stress disorder. A comprehensive clinical assessment allows clinicians to distinguish between these conditions by examining symptom duration, severity, triggers, and functional impairment.
Accurate diagnosis is essential because it directly influences treatment selection, prognosis, and service provision. Research indicates that structured diagnostic procedures and standardized assessment tools significantly improve diagnostic accuracy compared to unstructured clinical judgment alone (Garb, 2005). Thus, clinical assessment plays a vital role in ensuring that diagnostic decisions are evidence-based, ethically sound, and clinically meaningful.
2. Understanding the Whole Person Beyond Symptoms: Clinical assessment in psychology extends beyond the identification of disorders to achieve a holistic understanding of the individual. Psychological symptoms do not occur in isolation; they are embedded within a person’s biological makeup, psychological processes, social relationships, and cultural context. The bio-psychosocial model emphasizes that mental health problems arise from the interaction of these multiple factors rather than from a single cause (Engel, 1977).
Through comprehensive assessment, clinicians explore developmental history, family dynamics, educational and occupational functioning, personality traits, coping strategies, and life stressors. For instance, two individuals presenting with similar anxiety symptoms may differ significantly in terms of personality structure, trauma history, or social support. Clinical assessment enables psychologists to understand these individual differences and how they shape the expression and maintenance of psychological distress (Groth-Marnat & Wright, 2016).
This broader understanding also supports culturally responsive practice. Assessments that consider cultural values, beliefs, and norms help prevent misinterpretation of behaviors and reduce diagnostic bias. By focusing on the whole person rather than merely a checklist of symptoms, clinical assessment fosters empathy, strengthens the therapeutic alliance, and promotes more meaningful clinical formulations.
3. Guiding Individualized Treatment Planning: Another essential role of clinical assessment is its contribution to individualized and effective treatment planning. Assessment findings provide the foundation for selecting appropriate therapeutic approaches, setting treatment goals, and determining the intensity and duration of intervention. Rather than applying a one-size-fits-all model, clinicians use assessment data to tailor treatment to the client’s specific needs and circumstances (Norcross & Wampold, 2018).
For example, assessment may reveal that a client with depressive symptoms also experiences significant cognitive distortions and avoidance behaviors, suggesting that cognitive-behavioral therapy may be particularly beneficial. Alternatively, a history of unresolved trauma identified during assessment may indicate the need for trauma-focused interventions. Clinical assessment also helps identify potential barriers to treatment, such as low motivation, limited social support, or comorbid conditions, allowing clinicians to address these challenges proactively.
Research highlights that treatment outcomes improve when interventions are matched to client characteristics and preferences, a principle known as treatment responsiveness (Norcross & Wampold, 2018). In this way, clinical assessment acts as a roadmap for therapy, ensuring that treatment decisions are grounded in empirical evidence while remaining sensitive to the unique experiences of each individual.
4. Monitoring Treatment Progress and Outcomes: Clinical assessment plays a crucial role in monitoring treatment progress and evaluating therapeutic outcomes. Psychological treatment is a dynamic process, and clients may respond differently to interventions over time. Repeated assessment allows clinicians to systematically track changes in symptoms, functioning, and well-being, ensuring that treatment remains effective and responsive to the client’s needs (Lambert, 2013).
Outcome monitoring often involves the use of standardized symptom measures, session-by-session feedback tools, and periodic clinical evaluations. These assessments provide objective data that complement clinical observations and client self-reports. For example, a reduction in depression scale scores over time may indicate therapeutic improvement, while stagnant or worsening scores may signal the need for treatment modification.
Research consistently shows that routine outcome monitoring enhances treatment effectiveness and reduces the likelihood of client deterioration (Lambert, 2013). By using assessment as an ongoing feedback mechanism, psychologists can make informed decisions, strengthen collaborative care, and ensure that therapeutic goals are being achieved.
5. Supporting Risk Assessment and Safety Planning: A vital function of clinical assessment in psychology is identifying and managing risk. Psychologists are ethically and professionally responsible for assessing potential risks related to suicide, self-harm, violence, or neglect. Through careful clinical assessment, practitioners evaluate risk factors such as previous attempts, current ideation, emotional distress, substance use, and environmental stressors (Pisani et. al., 2011).
Risk assessment is not limited to identifying danger; it also involves evaluating protective factors, including social support, coping skills, and access to care. This balanced approach enables clinicians to develop effective safety plans tailored to the individual’s level of risk. For example, a client expressing suicidal ideation may require immediate intervention, increased monitoring, or referral to emergency services.
Clinical assessment in risk management is an ongoing process rather than a single event. Regular reassessment helps clinicians respond to changes in risk levels and maintain client safety. Effective risk assessment supports ethical practice, protects human life, and reinforces the psychologist’s duty of care (Pisani et. al., 2011).
6. Enhancing Clinical Decision-Making: Clinical assessment significantly enhances professional judgment and decision-making in psychological practice. While clinical intuition plays a role in therapy, relying solely on subjective impressions increases the risk of bias and error. Structured and evidence-based assessment methods provide a more reliable foundation for clinical decisions (Garb, 2005).
By integrating data from interviews, psychological tests, behavioral observations, and collateral reports, clinicians develop well-supported case formulations. These formulations guide decisions related to diagnosis, treatment selection, referral, and termination of therapy. Research has shown that clinicians who use structured assessment approaches make more accurate diagnostic and treatment decisions than those relying solely on unstructured judgment (Garb, 2005).
Clinical assessment also promotes transparency and accountability in practice. Decisions grounded in assessment data can be clearly explained to clients, supervisors, and other professionals, strengthening interdisciplinary collaboration and ethical responsibility.
7. Identifying Strengths and Protective Factors: Although clinical assessment is often associated with identifying problems and pathology, an equally important role is the identification of strengths and protective factors. A balanced assessment recognizes not only vulnerabilities but also the personal, social, and psychological resources that help individuals cope with adversity. These strengths may include resilience, problem-solving skills, supportive relationships, personal values, or past successful coping strategies (Snyder et. al., 2011).
By systematically assessing strengths, psychologists can shift the clinical focus from a deficit-based model to a more empowering and recovery-oriented approach. For example, identifying strong family support or high motivation for change can significantly influence treatment planning and prognosis. Strength-based assessment also enhances client engagement by validating their abilities and reinforcing hope.
Research in positive psychology emphasizes that integrating strengths into clinical work improves therapeutic alliance and treatment outcomes (Snyder et. al., 2011). Thus, clinical assessment plays a vital role in fostering resilience and promoting psychological well-being, not merely reducing symptoms.
8. Informing Prognosis and Long-Term Planning: Clinical assessment contributes significantly to understanding an individual’s prognosis and long-term mental health trajectory. Prognosis involves estimating the likely course, duration, and outcome of psychological difficulties based on multiple assessment variables, such as symptom severity, comorbidity, personality features, treatment history, and environmental supports (Beutler & Harwood, 2000).
Through comprehensive assessment, clinicians can anticipate potential challenges, such as relapse risk or treatment resistance, and plan accordingly. For instance, the presence of chronic stressors or limited social support may suggest the need for longer-term or more intensive intervention. Conversely, strong coping skills and early symptom improvement may indicate a favorable prognosis.
This role of clinical assessment helps clients and families develop realistic expectations and make informed decisions about treatment, education, and occupational planning. It also assists clinicians in determining appropriate levels of care, follow-up frequency, and preventative strategies.
9. Supporting Research and Evidence-Based Practice: Clinical assessment is fundamental to the advancement of research and evidence-based practice in psychology. Standardized assessment tools provide reliable and valid measures of psychological constructs, enabling researchers to evaluate treatment effectiveness, compare interventions, and refine theoretical models (Kazdin, 2008).
In clinical settings, assessment data allow practitioners to apply research findings to individual cases, bridging the gap between science and practice. Evidence-based practice relies on the integration of the best available research, clinical expertise, and client characteristics; an integration made possible through systematic assessment (Kazdin, 2008).
Without rigorous clinical assessment, psychological research would lack consistency and clinical practice would risk becoming anecdotal. Therefore, assessment serves as the backbone of scientifically grounded psychological care.
10. Upholding Ethical and Professional Standards: Clinical assessment plays a central role in maintaining ethical integrity and professional accountability in psychological practice. Ethical guidelines emphasize that psychologists must base their conclusions, diagnoses, and interventions on adequate and appropriate assessment procedures rather than on limited or subjective impressions (American Psychological Association, 2017). Through systematic assessment, clinicians demonstrate competence, responsibility, and respect for the individuals they serve.
Ethical clinical assessment involves obtaining informed consent, selecting assessment tools that are valid and reliable, and ensuring that instruments are used within the boundaries of the clinician’s training and expertise. Additionally, psychologists must consider cultural, linguistic, and contextual factors to avoid biased interpretations and unfair conclusions. Failure to conduct appropriate assessment can lead to misdiagnosis, ineffective treatment, and ethical violations (Groth-Marnat & Wright, 2016).
Clinical assessment also supports transparency and defensibility in professional decision-making. Well-documented assessment data allow psychologists to clearly justify their clinical judgments to clients, supervisors, courts, and other professionals when required. In this way, assessment not only guides clinical work but also safeguards the rights, dignity, and well-being of clients, reinforcing public trust in the profession of psychology (American Psychological Association, 2017).
In conclusion, Clinical assessment is far more than a diagnostic tool; it is a core process that underpins effective psychological practice. From understanding the individual and guiding treatment to managing risk and supporting ethical decision-making, assessment informs every stage of clinical work. Its multi-method, collaborative, and evolving nature reflects the complexity of human behavior and mental health. In an era increasingly focused on evidence-based and person-centered care, the role of clinical assessment remains indispensable. When conducted thoughtfully and ethically, clinical assessment not only enhances clinical outcomes but also strengthens the scientific integrity and humanistic values of psychology as a discipline.
Frequently Asked Questions (FAQs):
What is clinical assessment in psychology?
Clinical assessment is a systematic process used by psychologists to understand an individual’s mental health, behavior, emotions, and functioning. It involves tools like interviews, tests, observations, and questionnaires to guide diagnosis and treatment.
Why is clinical assessment important?
It helps psychologists accurately diagnose psychological disorders, understand the whole person, plan individualized treatment, monitor progress, manage risk, and make evidence-based decisions.
How does clinical assessment help in treatment planning?
Assessment identifies the client’s specific symptoms, strengths, and challenges. This information allows clinicians to choose the most appropriate therapy, set goals, and tailor interventions to the individual.
Can clinical assessment predict the outcome of therapy?
Yes, by evaluating factors like symptom severity, coping skills, support systems, and personality traits, psychologists can provide an informed prognosis and anticipate potential challenges during treatment.
What methods are used in clinical assessment?
Common methods include structured interviews, standardized psychological tests, behavioral observations, self-report questionnaires, and gathering information from family or other professionals.
How does clinical assessment address safety and risk?
Assessment helps identify risks like suicide, self-harm, or aggression and enables psychologists to create safety plans or interventions to protect the client and others.
Does clinical assessment focus only on problems?
No, modern clinical assessment also identifies strengths, coping skills, and protective factors, which can support resilience and improve treatment outcomes.
Is clinical assessment a one-time process?
No, it is ongoing. Psychologists reassess clients regularly to monitor progress, adjust treatment strategies, and ensure interventions remain effective.
How is clinical assessment connected to research?
Assessment data support evidence-based practice by providing measurable outcomes, guiding research studies, and helping translate findings into clinical interventions.
Are ethical guidelines important in clinical assessment?
Absolutely, psychologists must follow ethical standards, use valid tools, consider cultural factors, and ensure informed consent to protect clients and maintain professional accountability.
References:
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
- American Psychological Association. (2017). Ethical principles of psychologists and code of conduct (2003, amended effective June 1, 2010, and January 1, 2017). https://www.apa.org/ethics/code
- Beutler, L. E., & Harwood, T. M. (2000). Prescriptive psychotherapy: A practical guide to systematic treatment selection. Oxford University Press. https://doi.org/10.1093/med:psych/9780195136692.001.0001
- Engel G. L. (1977). The need for a new medical model: a challenge for biomedicine. Science (New York, N.Y.), 196(4286), 129–136. https://doi.org/10.1126/science.847460
- Garb, H. N. (2005). Clinical judgment and decision making. Annual Review of Clinical Psychology, 1(1), 67–89. https://doi.org/10.1146/annurev.clinpsy.1.102803.143810
- Groth-Marnat, G., & Wright, A. J. (2016). Handbook of psychological assessment (6th ed.). Wiley.
- Kazdin, A. E. (2008). Evidence-based treatment and practice: New opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist, 63(3), 146–159. https://doi.org/10.1037/0003-066X.63.3.146
- Lambert M. J. (2013). Outcome in psychotherapy: the past and important advances. Psychotherapy (Chicago, Ill.), 50(1), 42–51. https://doi.org/10.1037/a0030682
- Norcross, J. C., & Wampold, B. E. (2018). A new therapy for each patient: Evidence-based relationships and responsiveness. Journal of Clinical Psychology, 74(11), 1889–1906. https://doi.org/10.1002/jclp.22678
- Pisani, A. R., Cross, W. F., & Gould, M. S. (2011). The assessment and management of suicide risk: state of workshop education. Suicide & life-threatening behavior, 41(3), 255–276. https://doi.org/10.1111/j.1943-278X.2011.00026.x
- Snyder, C. R., Lopez, S. J., & Pedrotti, J. T. (2011). Positive psychology: The scientific and practical explorations of human strengths (2nd ed.). SAGE Publications.

Library Lecturer at Nurul Amin Degree College