An Overview of Acceptance and Commitment Therapy (ACT):
Acceptance and Commitment Therapy (ACT) is a form of psychotherapy that combines aspects of behavioral therapy and mindfulness to enhance psychological flexibility. Rather than attempting to eliminate difficult feelings, ACT encourages individuals to accept these experiences and commit to actions that align with their personal values. This approach helps individuals live meaningful lives despite the presence of emotional pain or distress. In the rest of this article, we will explore an overview of Acceptance and Commitment Therapy (ACT).
Core Processes of ACT:
ACT is built around six interconnected core processes that form a model aimed at enhancing psychological flexibility—the ability to be present, open, and committed to behavior that is aligned with personal values, even in the face of difficult experiences (Hayes, Strosahl, & Wilson, 1999). These processes are often represented through the “hexaflex” model, which illustrates their synergy rather than a linear progression. Each process contributes uniquely to the therapeutic goal of helping individuals live rich and meaningful lives while accepting the inevitable pain that life involves.
1. Acceptance: Acceptance in ACT refers to the active and conscious embracing of one’s private experiences, such as thoughts, emotions, memories, and bodily sensations—particularly those that are unpleasant—without attempting to escape, avoid, or suppress them (Hayes et al., 1999).
Conceptual Background: Unlike traditional approaches that emphasize control over negative internal experiences, ACT posits that experiential avoidance (i.e., efforts to suppress or avoid inner discomfort) is a major contributor to psychological distress. Instead, acceptance promotes openness to experiencing emotions as they are.
Practical Example: A client with panic disorder may learn to allow the sensations of a panic attack (racing heart, shortness of breath) to be present without struggling against them, thereby reducing the attack’s intensity over time.
Therapeutic Techniques:
- Mindfulness exercises
- Willingness metaphors (e.g., the “quicksand” metaphor)
- Experiential exposure to feared thoughts and feelings
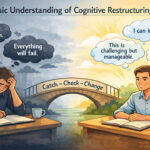
2. Cognitive Defusion: Cognitive defusion involves changing the way individuals relate to their thoughts, rather than trying to change the content of the thoughts themselves. It is the process of distancing oneself from thoughts by recognizing them as just words or mental events (Hayes, Luoma, Bond, Masuda, & Lillis, 2006).
Conceptual Background: In contrast to cognitive restructuring in traditional CBT, which aims to challenge and change maladaptive thoughts, ACT emphasizes that the literal believability of a thought is often less important than how much control it has over behavior.
Practical Example: Instead of reacting to the thought “I’m a failure” as if it were an absolute truth, the client might practice saying, “I’m having the thought that I’m a failure,” helping them create psychological space and reduce its impact.
Therapeutic Techniques:
- Thought labeling (“I’m having the thought that…”)
- Singing negative thoughts to silly tunes
- Using visual imagery to observe thoughts floating like clouds
3. Being Present (Contact with the Present Moment): This process encourages ongoing, flexible contact with the present moment, as opposed to being caught up in past regrets or future worries. It involves non-judgmental awareness and mindfulness (Hayes et al., 2012).
Conceptual Background: ACT views present-moment awareness as foundational for all other processes. When individuals are fully aware of the now, they are better able to respond to situations in a value-consistent way rather than reacting automatically or out of habit.
Practical Example: A person dealing with depression may learn to engage mindfully in everyday tasks like washing dishes or walking, instead of ruminating on past failures or future anxieties.
Therapeutic Techniques:
- Mindful breathing
- Body scan
- Grounding exercises using the five senses
4. Self-as-Context (The Observing Self): Self-as-context refers to the ability to observe one’s own inner experiences (thoughts, feelings, sensations) without being defined by them. It differentiates the “thinking self” (self-content) from the “observing self” (the consistent, unchanging awareness of one’s experience) (Hayes et al., 1999).
Conceptual Background: This process helps clients gain a perspective where they recognize that they are not the sum of their experiences or identities—they are the container in which those experiences occur. This promotes flexibility and decreases attachment to rigid self-concepts (e.g., “I’m broken”).
Practical Example: A trauma survivor might feel haunted by labels like “victim” or “damaged,” but learning to experience the self as a context can foster a more empowering identity—“I am the awareness behind these experiences, not the experiences themselves.”
Therapeutic Techniques:
- Perspective-taking exercises
- Observing thoughts without judgment
- “Chessboard” metaphor (pieces vs. the board)
5. Values: Values are chosen life directions—freely chosen, verbally constructed reinforcers that serve as a compass for meaningful living. They are not goals that can be completed, but enduring qualities of action that guide behavior (Dahl, Wilson, & Nilsson, 2004).
Conceptual Background: ACT asserts that values are central to psychological well-being. When individuals clarify what truly matters to them, they can persist through discomfort to live meaningfully.
Practical Example: A client may identify “compassion” as a core value and choose to volunteer, even when feeling socially anxious, because it aligns with this value.
Therapeutic Techniques:
- Values clarification worksheets
- Life compass or values card sort
- Reflective journaling on meaningful actions
6. Committed Action: Committed action is the process of setting goals guided by values and persistently working toward them, even in the face of difficulty. It involves building patterns of effective behavior over time (Hayes et al., 2012).
Conceptual Background: While acceptance and mindfulness create space, committed action propels clients forward toward behavioral change. It requires flexibility, courage, and willingness.
Practical Example: Someone who values connection might commit to calling a friend once a week, even though they feel lonely or awkward.
Therapeutic Techniques:
- SMART goal setting (Specific, Measurable, Achievable, Relevant, Time-bound)
- Behavior tracking
- Action planning with accountability
Integration Through the “Hexaflex”: The six core processes are often visualized as a hexaflex, where each point interacts with and supports the others. For example, committed action is difficult without value clarity, and acceptance is more sustainable when the person is grounded in the present moment. Together, these processes help clients develop psychological flexibility, the central aim of ACT (Hayes et al., 2006).
The Role of Mindfulness in ACT:
Mindfulness is a cornerstone of ACT, serving as both a process and a skill set that supports the development of psychological flexibility—the central aim of ACT. Mindfulness in ACT is not taught as an isolated meditation practice but is interwoven into therapeutic interventions that promote open, aware, and engaged ways of living (Hayes, Strosahl, & Wilson, 2012). Rather than eliminating negative thoughts or feelings, mindfulness helps individuals change their relationship with those experiences by cultivating non-judgmental awareness, acceptance, and present-moment focus. It encourages clients to observe their internal experiences without becoming entangled in them, thus enhancing their ability to act in alignment with personal values (Kabat-Zinn, 2005; Hayes et al., 2006).
1. Enhancing Present-Moment Awareness: A central function of mindfulness in ACT is to anchor individuals in the here and now. ACT posits that much of human suffering stems from excessive engagement with the past (e.g., guilt, regret) or the future (e.g., worry, fear), which pulls attention away from the current moment where meaningful action occurs (Hayes, Strosahl, & Wilson, 1999). Mindfulness counters this by training individuals to consciously observe thoughts, emotions, and surroundings as they unfold, moment to moment.
Theoretical Foundation: This emphasis on present-moment awareness stems from both behavioral psychology and Eastern contemplative practices, reinterpreted in ACT through a functional contextual lens. It enables psychological flexibility, the ability to respond adaptively to current demands rather than react habitually (Hayes et al., 2006).
Practical Example: A student facing academic stress may find themselves ruminating on past mistakes (“I failed last semester”) or worrying about future outcomes (“What if I flunk out?”). Through mindfulness, the student can learn to bring awareness back to what they are doing now, such as preparing for an exam or reading a textbook, thereby reducing overwhelm and increasing effectiveness.
Research Support: Shapiro et al. (2006) found that mindfulness enhances present-centered awareness, which directly contributes to improved emotional regulation, concentration, and wellbeing.
2. Supporting Acceptance of Difficult Emotions: Mindfulness enables individuals to observe emotional experiences without judgment, resistance, or attempts to suppress them. In ACT, this approach to emotional openness is termed acceptance—a willingness to experience emotions fully, precisely as they are, instead of engaging in experiential avoidance (Hayes et al., 2012).
Theoretical Foundation: ACT argues that emotional avoidance often intensifies suffering. For example, suppressing anxiety may lead to panic; avoiding sadness can foster depression. Mindfulness, when practiced consistently, teaches individuals to “sit with” emotions—recognizing them as temporary, passing experiences rather than threats that must be escaped (Fletcher & Hayes, 2005).
Practical Example: A person grieving the loss of a loved one might initially try to avoid sadness by staying constantly busy. In therapy, they learn to mindfully observe their grief—its physical sensations (tight chest), associated thoughts (“I miss them”), and feelings—without trying to alter or avoid them. This acceptance facilitates healing.
Research Support: Baer (2003) notes that acceptance, supported by mindfulness, leads to lower anxiety, depression, and stress by interrupting maladaptive avoidance patterns.
3. Facilitating Cognitive Defusion: Mindfulness helps people detach from unhelpful thoughts, a process ACT calls cognitive defusion. Rather than arguing with or suppressing thoughts, mindfulness teaches clients to observe them as thoughts, not truths or commands. This change in perspective reduces their influence on behavior (Hayes et al., 2006).
Theoretical Foundation: ACT holds that fusion—being entangled with thoughts—is a core contributor to psychological distress. For instance, the thought “I’m not good enough” becomes problematic when it’s believed as an absolute truth. Mindfulness introduces defusion techniques that help individuals observe these thoughts from a distance, weakening their control.
Practical Example: A client with social anxiety might think, “Everyone will laugh at me.” Through mindful defusion, they learn to notice the thought, label it (“I’m having the thought that…”), and refocus on valued behavior, such as giving a presentation despite discomfort.
Research Support: Studies show that mindfulness-based defusion decreases the believability and distress associated with negative self-statements (Masuda et al., 2004).
4. Cultivating Self-as-Context: Mindfulness supports the ACT process of self-as-context, also known as the observing self. This involves recognizing that one is not the content of their experiences (e.g., thoughts, feelings, roles), but rather the awareness behind them. It’s the stable perspective from which all experiences are noticed (Hayes et al., 2012).
Theoretical Foundation: Traditional self-concepts (e.g., “I am a failure”) are rigid and often linked to suffering. ACT uses mindfulness to shift identity from these narrative selves to a broader, more flexible perspective—where one notices experiences without becoming them. This fosters resilience, particularly in trauma, depression, or chronic pain.
Practical Example: A combat veteran may say, “I am broken because of what I’ve seen.” Mindfulness practices can help the veteran observe these thoughts and feelings without identifying with them, discovering that the self is not broken—it is the witness of experience.
Research Support: Fletcher and Hayes (2005) explain that mindfulness enhances perspective-taking and reduces attachment to rigid self-concepts, promoting emotional stability and growth.
5. Increasing Emotional Regulation: While ACT does not aim to eliminate emotions, mindfulness significantly improves one’s ability to manage them. By learning to pause, observe, and accept emotions, individuals gain greater emotional regulation, reducing impulsive reactions and promoting values-based actions (Baer, 2003).
Theoretical Foundation: Emotions are seen not as problems, but as transient events that can be observed with curiosity. Mindfulness increases awareness of emotional patterns, physiological cues, and triggers, enabling a space between stimulus and response—a key to intentional living (Hayes et al., 1999).
Practical Example: A person with anger issues might notice early signs of tension (clenched fists, heat rising) and use mindful breathing to ground themselves before reacting aggressively. This pause allows them to respond in a way that aligns with their values (e.g., respect, calm).
Research Support: Mindfulness practices have been shown to activate the prefrontal cortex and reduce amygdala reactivity, mechanisms associated with better emotion regulation (Chiesa & Serretti, 2009).
6. Strengthening Behavioral Flexibility: Mindfulness encourages clients to act in accordance with their chosen values, even in the presence of uncomfortable internal experiences like fear, pain, or uncertainty. This capacity is known in ACT as committed action, which relies on behavioral flexibility—the ability to choose responses based on personal meaning, rather than automatic emotional or cognitive reactions (Hayes et al., 2012).
Theoretical Foundation: ACT integrates principles of functional contextualism, which focus on how behaviors function in context. Mindfulness allows individuals to recognize when they are acting out of habit or avoidance and instead respond in ways that serve their long-term goals (Hayes et al., 1999).
Practical Example: A person with a fear of public speaking values sharing knowledge. Through mindfulness, they notice fear without reacting to it and choose to give a presentation anyway, thus strengthening their commitment to growth and leadership.
Research Support: Mindfulness supports this by disrupting habitual avoidance and reinforcing deliberate, values-based behavior (Levin et al., 2012).
7. Enhancing Attention and Focus: Mindfulness strengthens attentional control—the ability to focus, sustain, and shift attention deliberately. In ACT, attentional flexibility is crucial because it empowers individuals to disengage from self-defeating thoughts and instead attend to the task at hand or personal values (Shapiro et al., 2006).
Theoretical Foundation: Distraction and mind-wandering often correlate with lower well-being and reduced performance. ACT uses mindfulness techniques such as focused breathing and observing thoughts to stabilize attention, which increases cognitive efficiency and emotional clarity (Chambers, Gullone, & Allen, 2009).
Practical Example: A person with ADHD who often gets distracted during work uses short, daily mindfulness practices to improve their ability to notice when their mind wanders and gently bring it back to the task.
Research Support: Studies indicate that regular mindfulness training improves executive attention, working memory, and task performance (Tang et al., 2007).
8. Promoting Nonjudgmental Awareness: Mindfulness cultivates nonjudgmental awareness, allowing clients to observe their thoughts, emotions, and bodily sensations without labeling them as “bad,” “good,” “weak,” or “unacceptable.” This creates emotional neutrality and fosters psychological openness (Kabat-Zinn, 2005).
Theoretical Foundation: In ACT, judgment often contributes to psychological inflexibility. For instance, judging oneself for feeling anxious often leads to shame or avoidance. Mindfulness creates a space where experiences are allowed to “just be,” reducing secondary emotional suffering (Hayes et al., 2006).
Practical Example: A person with body image issues might normally respond to critical thoughts like “I look awful” with self-loathing. Mindfulness helps them notice such thoughts without judgment, reducing the emotional charge and the tendency to withdraw socially.
Research Support: Baer et al. (2006) found that nonjudgmental acceptance, a core element of mindfulness, was significantly associated with lower levels of anxiety and depression.
9. Grounding the Client in the Therapeutic Process: Mindfulness is often used as a gateway technique in ACT sessions to help clients tune into their internal experience and become present. This grounding prepares them for therapeutic work by reducing cognitive overload and promoting a calm, open attitude.
Theoretical Foundation: ACT therapists frequently start sessions with short mindfulness practices such as body scans, breathing exercises, or “noticing the room.” This prepares the client to access deeper material and respond with less defensiveness or avoidance (Fletcher & Hayes, 2005).
Practical Example: A therapist might begin a session with a minute of mindful breathing. This helps a client who arrives feeling rushed or scattered to center themselves, making the session more productive and emotionally safe.
Research Support: Mindfulness-based grounding practices are shown to enhance therapeutic rapport and increase client openness (Germer, Siegel, & Fulton, 2016).
10. Enhancing Compassion Toward Self and Others: ACT integrates mindfulness to promote self-compassion and empathy, helping clients respond to suffering with kindness rather than self-criticism or blame. This is especially important in overcoming shame, guilt, or interpersonal conflict (Neff, 2003).
Theoretical Foundation: Self-criticism is a major contributor to depression, anxiety, and low self-esteem. ACT challenges the narrative self and encourages the observing self to respond with warmth and understanding. Mindfulness allows clients to witness their struggles and treat themselves as they would a suffering friend (Hayes et al., 2012).
Practical Example: A perfectionistic student who fails a test might engage in harsh self-talk. With mindfulness and self-compassion practices, they learn to acknowledge disappointment while affirming their worth, leading to greater emotional balance and resilience.
Research Support: Self-compassion interventions grounded in mindfulness are linked to improved mental health, lower stress, and better relationship outcomes (Neff & Germer, 2013).
What Can ACT Therapy Help With?
ACT is a versatile, evidence-based approach that has shown effectiveness across a wide range of psychological, behavioral, and even physical health issues. Unlike therapies that aim to reduce or eliminate symptoms directly, ACT focuses on helping individuals live meaningful, value-driven lives while learning to accept and manage internal distress (Hayes, Strosahl, & Wilson, 2012). This transdiagnostic approach makes it applicable across many mental health conditions and contexts.
1. Anxiety Disorders: ACT has been widely applied to treat various anxiety disorders, including Generalized Anxiety Disorder (GAD), panic disorder, social anxiety, and specific phobias. These conditions often involve persistent fear, worry, and avoidance behaviors that interfere with daily functioning.
ACT’s Approach: Rather than attempting to eliminate anxious thoughts and feelings, ACT helps individuals accept anxiety as a natural part of life. Clients learn to distance themselves from anxious thoughts through cognitive defusion and commit to value-based actions even in the presence of fear (Eifert & Forsyth, 2005).
Example: An individual with social anxiety may experience thoughts like “Everyone will think I’m stupid.” Through ACT, they learn to notice the thought without judgment, allow the anxiety to be present, and still choose to attend social gatherings that align with their value of connection.
Supporting Research: Studies show ACT is as effective as Cognitive Behavioral Therapy (CBT) for anxiety, especially in reducing avoidance and enhancing quality of life (Arch et al., 2012).
2. Depression: Depression is characterized by persistent low mood, loss of interest, and negative thought patterns. People with depression often engage in experiential avoidance—efforts to suppress or escape from painful emotions, which paradoxically increase distress.
ACT’s Approach: ACT targets the fusion with negative self-narratives and promotes acceptance of painful emotions while encouraging individuals to take small, meaningful steps in line with their values (Hayes, Strosahl, & Wilson, 2012). The goal is not to feel better, but to live better, even with emotional pain.
Example: A person who feels “I’m useless” learns to observe that thought from a distance and still engages in valued actions, like volunteering or reconnecting with friends.
Supporting Research: ACT has been found effective for major depression and treatment-resistant depression, especially in increasing psychological flexibility, which predicts long-term recovery (Forman et al., 2007).
3. Chronic Pain and Medical Conditions: ACT has gained strong empirical support in the management of chronic pain and physical health conditions such as cancer, diabetes, multiple sclerosis, and fibromyalgia. Chronic conditions often bring not just physical pain, but emotional and social challenges.
ACT’s Approach: ACT encourages patients to stop struggling with pain and instead focus on building a meaningful life alongside the discomfort. Clients learn pain acceptance, defusion from pain-related thoughts, and engagement in life activities that reflect their values (Driscoll et. al., 2021).
Example: Someone with chronic back pain may reduce activity out of fear of aggravating the condition. ACT helps them mindfully engage in gradual activity, like walking with loved ones, aligned with their value of connection.
Supporting Research: ACT has shown consistent success in improving quality of life, physical functioning, and emotional well-being in chronic pain populations (Vowles & Thompson, 2011).
4. Obsessive-Compulsive Disorder (OCD): OCD involves persistent, intrusive thoughts (obsessions) and repetitive behaviors (compulsions) aimed at reducing distress. Traditional treatments involve exposure and response prevention (ERP), but ACT provides an alternative approach.
ACT’s Approach: Rather than suppressing or neutralizing obsessions, ACT teaches individuals to accept intrusive thoughts without engaging with them. Clients learn that thoughts do not need to dictate behavior and can commit to actions aligned with their values (Twohig et al., 2006).
Example: A person with contamination fears learns to touch a public doorknob, experience the anxiety without engaging in handwashing rituals, and refocus on their commitment to work or relationships.
Supporting Research: ACT has been shown to be effective in reducing OCD symptoms, especially in individuals who do not respond well to traditional ERP methods (Krafft et. al., 2022).
5. Trauma and Post-Traumatic Stress Disorder (PTSD): PTSD and trauma-related disorders involve reliving distressing memories, hypervigilance, avoidance, and emotional numbing. Traditional exposure-based therapies may be difficult for some trauma survivors.
ACT’s Approach: ACT provides an alternative by helping clients accept the presence of trauma-related memories and emotions without avoidance. By fostering mindfulness, defusion, and values-based action, clients move toward a meaningful life not defined by the trauma (Walser & Westrup, 2007).
Example: A military veteran with PTSD may learn to sit with painful flashbacks and engage in family activities aligned with their value of love, rather than isolate themselves out of fear.
Supporting Research: ACT-based trauma treatments have demonstrated strong outcomes in reducing PTSD symptoms, particularly emotional avoidance and experiential disconnection (Meyer et al., 2018).
6. Substance Use Disorders: Substance use disorders (SUDs) often involve avoiding painful emotions or memories by engaging in drug or alcohol use. Traditional treatments may emphasize abstinence and relapse prevention but can struggle with long-term maintenance, especially if emotional avoidance isn’t addressed.
ACT’s Approach: ACT helps individuals accept cravings and difficult emotions without acting on them. Rather than viewing cravings as enemies to be eliminated, clients learn to see them as temporary internal experiences that do not need to control behavior. ACT emphasizes aligning actions with long-term values such as health, relationships, or integrity (Hayes, Strosahl, & Wilson, 2012).
Example: A person recovering from alcohol dependence might use ACT skills to notice and accept a craving after a stressful day at work and choose to call a friend or go for a walk instead—supporting their value of staying connected and healthy.
Supporting Research: ACT has shown promise in treating substance use and promoting long-term recovery by enhancing psychological flexibility (Luoma, Kohlenberg, Hayes, Bunting, & Rye, 2008).
7. Eating Disorders and Body Image Issues: Eating disorders such as anorexia, bulimia, and binge eating disorder are often driven by rigid self-judgments, perfectionism, and avoidance of distressing emotions or bodily sensations. ACT provides a non-judgmental, values-based path toward healing.
ACT’s Approach: ACT helps clients accept distressing thoughts and emotions (like guilt or shame) about food, weight, or appearance rather than fight or avoid them. By practicing mindfulness and defusion, individuals can reconnect with their bodies in a more compassionate way and take action consistent with their values, such as self-care, health, or authenticity (Juarascio, Forman, & Herbert, 2010).
Example: A client with binge eating disorder learns to notice the urge to binge as a passing feeling and instead engages in a self-care activity like journaling or walking, aligned with the value of emotional honesty.
Supporting Research: ACT interventions have been shown to reduce disordered eating behaviors and body dissatisfaction while improving emotional regulation and self-compassion (Pearson et al., 2012).
8. Stress and Burnout: In today’s fast-paced world, workplace stress and burnout are increasingly common—especially in high-stakes fields like healthcare, education, and law enforcement. Chronic stress can lead to emotional exhaustion, reduced performance, and even depression.
ACT’s Approach: ACT addresses burnout by helping individuals clarify personal values, reduce experiential avoidance, and adopt a mindful stance toward stressors. Through psychological flexibility, clients learn to stay engaged with meaningful work even when pressure or fatigue arises (Lloyd, Bond, & Flaxman, 2013).
Example: A teacher feeling overwhelmed by job demands learns to notice stress without judgment and reconnects with their original value of supporting students, helping them feel reinvigorated and less reactive to daily frustrations.
Supporting Research: ACT-based interventions in the workplace have led to improvements in job satisfaction, mental health, and work engagement, especially among individuals at high risk of burnout (Flaxman & Bond, 2010).
9. Relationship Problems: Interpersonal conflict, miscommunication, and emotional disconnection can damage relationships over time. These issues often stem from reactivity to emotions, rigid thinking, or attempts to control the behavior of others.
ACT’s Approach: ACT enhances relationship functioning by promoting emotional acceptance, mindful listening, and values-based communication. Individuals are taught to let go of the struggle to “fix” others and instead focus on living according to values like honesty, kindness, and respect (Jacobson et al., 2000).
Example: In couples therapy, one partner may learn to accept difficult emotions like jealousy or insecurity without acting on them impulsively, choosing instead to communicate openly and lovingly.
Supporting Research: ACT-informed couple interventions have shown positive outcomes in conflict resolution, intimacy, and long-term relationship satisfaction (Cordova, 2001).
10. Non-Clinical Applications: Enhancing Performance and Well-Being: ACT is not just for clinical populations—it is also used to enhance performance, resilience, and well-being in non-clinical settings such as sports, education, business, and personal development.
ACT’s Approach: The core process of psychological flexibility—the ability to be open, present, and engaged in meaningful action—is beneficial in high-performance environments. ACT helps individuals handle pressure, stay focused, and align performance with core values, rather than chasing perfection or avoiding failure (Gardner & Moore, 2007).
Example: An athlete struggling with pre-game anxiety learns to allow the nervous energy to be there while maintaining focus on their goal: playing with courage and teamwork.
Supporting Research: ACT interventions have been effective in improving academic performance, leadership effectiveness, athletic performance, and overall life satisfaction (Kashdan & Rottenberg, 2010; Ruiz, 2010).
How Effective Is ACT?
ACT has emerged as one of the most influential and empirically supported forms of psychotherapy in contemporary clinical psychology. Grounded in behavioral science, ACT focuses on cultivating psychological flexibility, a skill that enables individuals to accept unpleasant experiences while committing to value-based actions (Hayes, Strosahl, & Wilson, 1999, 2012). Over the past two decades, numerous randomized controlled trials, meta-analyses, and longitudinal studies have explored ACT’s effectiveness, confirming its benefits across a wide array of psychological and physical conditions.
1. Empirical Evidence Across Mental and Physical Health Conditions: ACT has demonstrated effectiveness across a wide spectrum of psychological disorders and physical health issues, including depression, anxiety, psychosis, substance use, chronic pain, and stress-related disorders.
A-Tjak et al. (2015) conducted a meta-analysis of 39 randomized controlled trials (RCTs) and found a moderate overall effect size for ACT (Cohen’s d = 0.68), which is on par with or superior to many standard psychotherapies.
Gloster et al. (2020) reviewed multiple meta-analyses and concluded that ACT has comparable efficacy to CBT, particularly in promoting well-being and life satisfaction, not just symptom relief.
2. Comparative Effectiveness with CBT and Other Therapies: ACT shares similarities with Cognitive Behavioral Therapy (CBT) but diverges in its goal: rather than changing thoughts, ACT helps individuals accept them while focusing on committed actions rooted in values. This fundamental shift offers unique benefits.
In a landmark comparative trial by Forman et al. (2007), both ACT and CBT significantly reduced depression and anxiety symptoms. However, ACT led to greater improvements in quality of life and value-based living, even when symptom reduction was similar.
McLoughlin & Roche (2023) found that ACT was as effective as CBT in treating OCD, PTSD, and social anxiety disorder, with lower dropout rates and higher levels of patient satisfaction.
3. Durability of Treatment Effects and Long-Term Benefits: A hallmark of ACT is that its effects are long-lasting. This is attributed to its emphasis on psychological flexibility, which equips individuals with tools they can apply beyond therapy sessions.
Fledderus et al. (2012) found that individuals who received ACT-based interventions showed significant improvements in depression and well-being that lasted through 6- and 12-month follow-ups.
Ciarrochi et al. (2011) demonstrated in a longitudinal study that improvements in psychological flexibility during adolescence predicted greater emotional resilience and academic success years later.
4. ACT in Physical Health and Chronic Illness: ACT is also widely applied in chronic health conditions, where the emphasis is not only on symptom reduction but also improving functioning and quality of life despite ongoing symptoms.
McCracken (2020) used ACT to treat patients with chronic pain, resulting in improved functioning and reduced disability, even when pain levels remained constant.
For patients with diabetes, cancer, and multiple sclerosis, ACT has been effective in promoting adherence to treatment, emotional regulation, and improved life satisfaction (Graham et al., 2016).
5. Digital Delivery and Accessibility of ACT: One of ACT’s strengths is its versatility—it can be delivered in various formats: individual therapy, group therapy, workshops, and increasingly via digital interventions.
Spijkerman et al. (2016) conducted a meta-analysis of online mindfulness-based interventions and found significant improvements in mental health, suggesting ACT can be effectively delivered online.
Programs like ACT Companion, iACT, and web-based ACT have shown success in reducing stress, anxiety, and burnout among healthcare professionals and students.
6. Cost-Effectiveness and Scalability: ACT is not only effective but also cost-efficient, making it suitable for large-scale implementation in healthcare systems and organizational settings.
Ost (2014) highlighted that ACT’s cost per outcome improvement was equivalent or better than traditional therapies, particularly in group formats or self-help interventions.
ACT has also been integrated into employee wellness programs, where it improves job satisfaction, reduces absenteeism, and mitigates burnout (Flaxman & Bond, 2010).
7. Psychological Flexibility as a Transdiagnostic Mechanism: At the heart of ACT lies psychological flexibility, which is increasingly recognized as a transdiagnostic factor—a mechanism that underlies many different psychological disorders.
Kashdan and Rottenberg (2010) argued that psychological flexibility is critical to health and emotional well-being across life domains.
Interventions that increase this flexibility predict improved outcomes across conditions like depression, anxiety, trauma, and even physical illness.
Challenges & Limitations of ACT:
While ACT has garnered significant empirical support and clinical success, like all psychological interventions, it is not without challenges and limitations. These limitations may relate to aspects of its theoretical model, practical application, client suitability, or research evidence. Understanding these constraints is crucial for therapists, researchers, and policymakers when considering ACT for diverse populations and settings.
1. Conceptual Complexity and Theoretical Ambiguity: ACT is grounded in Relational Frame Theory (RFT), a contextual behavioral theory of language and cognition. While RFT provides a rich theoretical foundation, it is complex and difficult to understand for many clinicians, especially those trained in more traditional cognitive-behavioral approaches.
Some critics argue that RFT, though theoretically rigorous, is overly abstract and lacks clinical utility for most practitioners (Luciano et al., 2004).
Therapists new to ACT may find its non-linear processes, use of metaphors, and experiential techniques challenging to grasp and implement effectively.
2. Therapist Competence and Training Requirements: Unlike structured interventions like CBT, ACT places a high demand on the therapist’s interpersonal sensitivity, creativity, and experiential delivery skills. This can pose difficulties for clinicians who prefer more manualized or didactic treatment approaches.
The flexibility of ACT—while beneficial—also means it can be difficult to standardize, leading to inconsistencies in therapeutic delivery (Gaudiano, 2009).
Inadequate training can result in the misapplication of techniques, such as confusing acceptance with resignation or mindfulness with relaxation.
3. Suitability for Certain Clients and Populations: ACT may not be suitable for all clients, particularly those with low insight, severe cognitive impairments, or those seeking immediate symptom relief rather than value-based living.
Clients unfamiliar with abstract or metaphorical language may struggle to engage in ACT’s experiential exercises and metaphors (e.g., “the passengers on the bus” or “leaves on a stream”).
Individuals in acute crisis or psychotic states may find ACT’s introspective components too demanding unless carefully adapted.
4. Limited Research in Certain Clinical Populations: Although ACT’s evidence base is strong and growing, some specific clinical populations remain underrepresented in the literature, such as those with eating disorders, certain personality disorders, and severe neurodevelopmental disorders.
Longitudinal studies examining the durability of ACT effects across diverse cultural backgrounds are still relatively limited.
Comparative studies directly assessing ACT against gold-standard treatments in specific conditions (e.g., DBT for borderline personality disorder) are also fewer in number.
5. Misinterpretation of Core Concepts: A common limitation observed in the application of ACT is the misunderstanding or superficial application of core processes, particularly acceptance and defusion.
For instance, acceptance may be mistaken for passivity, leading clients to tolerate harmful situations (e.g., abuse) instead of making assertive value-based changes.
Similarly, cognitive defusion, when poorly applied, may result in clients disengaging from useful cognitive strategies or over-intellectualizing emotional experiences.
6. Cultural Limitations and Generalizability: ACT originated in Western contexts and may face limitations when applied across non-Western, collectivist, or religious populations, particularly where the individualistic emphasis on personal values might conflict with cultural norms.
The concept of “self-as-context” may be difficult to translate into languages or cultures that emphasize interconnectedness or external determinants of identity.
Adapting metaphors, value exercises, and mindfulness techniques in culturally sensitive ways remains a work in progress (Masuda et al., 2023).
7. Measurement Challenges and Lack of Standardization: ACT primarily measures treatment progress using psychological flexibility via instruments like the Acceptance and Action Questionnaire (AAQ-II). However, some scholars have raised concerns about the reliability, construct validity, and sensitivity of these tools.
Critics argue that self-report measures may overlap with constructs like distress tolerance or emotional regulation, leading to ambiguous interpretations (Tyndall et al., 2019).
There is also a need for more objective, behavioral outcome measures in ACT research.
8. Limited Visibility in Some Clinical Settings: Despite its growing popularity, ACT is still less well known or integrated in certain clinical systems compared to CBT, DBT, or psychodynamic therapies.
Insurance providers, hospital programs, and governmental health systems may not yet fully endorse or reimburse ACT-based treatments, limiting accessibility.
This lack of structural support can discourage clinicians from investing in ACT training and certification.
In conclusion, Acceptance and Commitment Therapy (ACT) represents a significant development in psychological treatment, offering a holistic approach that integrates mindfulness, acceptance, and value-driven action. Its foundation in functional contextualism and RFT provides a robust theoretical framework, while its core processes offer practical strategies for enhancing psychological flexibility. As research continues to support its efficacy across diverse populations and settings, ACT remains a vital and evolving component of contemporary psychotherapy.
Frequently Asked Questions (FAQs):
What is Acceptance and Commitment Therapy (ACT)?
Acceptance and Commitment Therapy (ACT) is a modern form of psychotherapy that helps people live more meaningful lives by teaching them how to accept their inner experiences and commit to actions that align with their personal values. Instead of trying to eliminate difficult thoughts or emotions, ACT focuses on changing how we relate to them so they have less power over our behavior.
How is ACT different from traditional cognitive behavioral therapy (CBT)?
Both ACT and CBT are effective approaches, but they differ in key ways. CBT typically aims to change unhelpful thoughts into more balanced ones. ACT, on the other hand, does not try to change thoughts but teaches people to accept them without letting them control their actions. ACT emphasizes mindfulness, acceptance, and personal values as the foundation for behavior change.
What kinds of problems can ACT help with?
ACT can help with a wide range of mental health and life challenges, including:
- Depression and anxiety
- Stress and burnout
- Chronic pain or illness
- Addictions and substance use
- Trauma and PTSD
- Eating disorders
- Low self-esteem
- Work and relationship difficulties
It’s also used to enhance general well-being, motivation, and personal growth, even in people without a mental health diagnosis.
Can ACT be used with children and teens?
Yes, ACT can be adapted for children and adolescents. When presented in age-appropriate language and with engaging activities or metaphors, young people can learn to become more aware of their thoughts and feelings, and take steps toward what matters most to them, like friendships, learning, or family connections.
How long does ACT therapy take?
The length of ACT therapy varies depending on a person’s goals and needs. Some people find benefits in a few sessions, while others may attend for several months. ACT is flexible and can be offered as brief interventions, weekly sessions, or even ongoing coaching. It can also be provided in individual, group, or online formats.
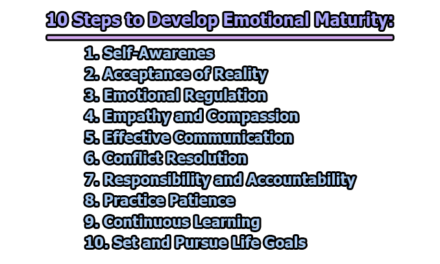
What are the six core processes in ACT?
ACT is based on six core processes that work together to build psychological flexibility:
- Acceptance – Opening up to uncomfortable thoughts and feelings without fighting them.
- Cognitive Defusion – Learning to observe thoughts without being dominated by them.
- Being Present – Staying mindful and connected to the current moment.
- Self-as-Context – Seeing yourself as more than just your thoughts or emotions.
- Values – Identifying what truly matters to you in life.
- Committed Action – Taking steps guided by your values, even when it’s hard.
Together, these help people respond more effectively to life’s challenges and move toward a meaningful life.
Can ACT be combined with other treatments?
Yes, ACT is often used alongside other approaches such as medication, traditional talk therapy, or behavioral strategies. It can also be blended with other therapies like Dialectical Behavior Therapy (DBT) or Motivational Interviewing. ACT is flexible and can enhance other forms of support by focusing on values and present-moment awareness.
Is ACT effective?
Yes, ACT has been shown to be effective for a variety of conditions and challenges. It is considered an evidence-based therapy, meaning it is supported by scientific studies and clinical trials. Many people find ACT especially helpful when they’ve tried other approaches that focused only on symptom reduction and want to build a more meaningful, values-driven life.
How can I find an ACT therapist?
You can find ACT therapists through therapy directories, professional mental health websites, or local counseling centers. Look for therapists who mention “Acceptance and Commitment Therapy” in their profiles or who specialize in mindfulness-based approaches. It’s also okay to ask a therapist directly about their experience with ACT during your first session or consultation.
References:
- A-Tjak, J. G., Davis, M. L., Morina, N., Powers, M. B., Smits, J. A., & Emmelkamp, P. M. (2015). A Meta-Analysis of the Efficacy of Acceptance and Commitment Therapy for Clinically Relevant Mental and Physical Health Problems. Psychotherapy & Psychosomatic, 84, 30-36. https://doi.org/10.1159/000365764
- Arch, J. J., & Craske, M. G. (2008). Acceptance and commitment therapy and cognitive behavioral therapy for anxiety disorders: Different treatments, similar mechanisms? Clinical Psychology: Science and Practice, 15(4), 263–279. https://doi.org/10.1111/j.1468-2850.2008.00137.x
- Arch, J. J., Eifert, G. H., Davies, C., Plumb, J. C., Rose, R. D., & Craske, M. G. (2012). Randomized Clinical Trial of Cognitive Behavioral Therapy (CBT) versus Acceptance and Commitment Therapy (ACT) for Mixed Anxiety Disorders. Journal of Consulting and Clinical Psychology, 80, 750-765. http://dx.doi.org/10.1037/a0028310
- Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143. https://doi.org/10.1093/clipsy.bpg015
- Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
- Chambers, R., Gullone, E., & Allen, N. B. (2009). Mindful emotion regulation: An integrative review. Clinical Psychology Review, 29(6), 560–572. https://doi.org/10.1016/j.cpr.2009.06.005
- Chiesa, A., & Serretti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: A review and meta-analysis. Journal of Alternative and Complementary Medicine, 15(5), 593–600. https://doi.org/10.1089/acm.2008.0495
- Ciarrochi, J., Kashdan, T. B., Leeson, P., Heaven, P., & Jordan, C. (2011). On being aware and accepting: A one-year longitudinal study into adolescent well-being. Journal of Adolescence, 34(4), 695–703. https://doi.org/10.1016/j.adolescence.2010.09.003
- Cordova, J. V. (2001). Acceptance in behavior therapy: Understanding the process of change. The Behavior Analyst, 24(2), 213–226. https://doi.org/10.1007/BF03392032
- Dahl, J., Wilson, K. G., & Nilsson, A. (2004). Acceptance and Commitment Therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behavior Therapy, 35(4), 785–802. https://doi.org/10.1016/S0005-7894(04)80020-0
- Driscoll, M. A., Edwards, R. R., Becker, W. C., Kaptchuk, T. J., & Kerns, R. D. (2021). Psychological Interventions for the Treatment of Chronic Pain in Adults. Psychological Science in the Public Interest, 22(2), 52-95. https://doi.org/10.1177/15291006211008157
- Eifert, G. H., & Forsyth, J. P. (2005). Acceptance and commitment therapy for anxiety disorders: A practitioner’s treatment guide to using mindfulness, acceptance, and values-based behavior change strategies. New Harbinger Publications.
- Fletcher, L., & Hayes, S. C. (2005). Relational Frame Theory, Acceptance and Commitment Therapy, and a functional analytic definition of mindfulness. Journal of Rational-Emotive and Cognitive-Behavior Therapy, 23(4), 315–336. https://doi.org/10.1007/s10942-005-0017-7
- Fledderus, M., Bohlmeijer, E. T., Pieterse, M. E., & Schreurs, K. M. (2012). Acceptance and commitment therapy as guided self-help for psychological distress and positive mental health: A randomized controlled trial. Psychological Medicine, 42(3), 485–495. https://doi.org/10.1017/S0033291711001206
- Forman, E.M., Herbert, J.D., Moitra, E., Yeomans, P.D. and Geller, P.A. (2007) A Randomized Controlled Effectiveness Trial of Acceptance and Commitment Therapy and Cognitive Therapy for Anxiety and Depression. Behavior Modification, 31, 772-799. https://doi.org/10.1177/0145445507302202
- Flaxman, P. E., & Bond, F. W. (2010). Worksite stress management training: Moderated effects and clinical significance. Journal of Occupational Health Psychology, 15(4), 347–358. https://doi.org/10.1037/a0020522
- Gardner, F. L., & Moore, Z. E. (2007). The Psychology of Enhancing Human Performance: The Mindfulness-Acceptance-Commitment (MAC) Approach. New York: Springer Publishing.
- Germer, C. K., Siegel, R. D., & Fulton, P. R. (2016). Mindfulness and Psychotherapy (2nd ed.). Guilford Press.
- Gloster, A. T., Walder, N., Levin, M. E., Twohig, M. P., & Karekla, M. (2020). The empirical status of acceptance and commitment therapy: A review of meta-analyses. Journal of Contextual Behavioral Science, 18, 181–192. https://doi.org/10.1016/j.jcbs.2020.09.009
- Gaudiano, B. A. (2009). Evaluating Acceptance and Commitment Therapy: An Analysis of a Recent Critique. International Journal of Behavioral Consultation and Therapy, 5(3-4), 311–329.
- Graham, C. D., Gouick, J., Krahé, C., & Gillanders, D. (2016). A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clinical Psychology Review, 46, 46–58. https://doi.org/10.1016/j.cpr.2016.04.009
- Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and Commitment Therapy: An experiential approach to behavior change. New York: Guilford Press.
- Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006
- Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). The Guilford Press.
- Hayes, S. C., Hofmann, S. G., & Ciarrochi, J. (2020). A process-based approach to psychological diagnosis and treatment: The conceptual and treatment utility of an extended evolutionary meta model. Clinical Psychology Review, 82, 101908. https://doi.org/10.1016/j.cpr.2020.101908
- Juarascio, A. S., Forman, E. M., & Herbert, J. D. (2010). Acceptance and commitment therapy versus cognitive therapy for the treatment of comorbid eating pathology. Behavior Modification, 34(2), 175–190. https://doi.org/10.1177/0145445510363472
- Jacobson, N. S., Christensen, A., Prince, S. E., Cordova, J., & Eldridge, K. (2000). Integrative behavioral couple therapy: An acceptance-based, promising new treatment for couple discord. Journal of Consulting and Clinical Psychology, 68(2), 351–355.
- Kabat-Zinn, J. (2005). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness (15th anniversary ed.). Delta Trade Paperback/Bantam Dell.
- Kashdan, T. B., & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878. https://doi.org/10.1016/j.cpr.2010.03.001
- Krafft, J., Petersen, J. M., & Twohig, M. P. (2022). Acceptance and commitment therapy for obsessive-compulsive and related disorders. In E. A. Storch, J. S. Abramowitz, & D. McKay (Eds.), Complexities in obsessive-compulsive and related disorders: Advances in conceptualization and treatment (pp. 352–369). Oxford University Press. https://doi.org/10.1093/med-psych/9780190052775.003.0019
- Levin, M. E., Hildebrandt, M. J., Lillis, J., & Hayes, S. C. (2012). The impact of treatment components suggested by the psychological flexibility model: A meta-analysis of laboratory-based component studies. Behavior Therapy, 43(4), 741–756. https://doi.org/10.1016/j.beth.2012.05.003
- Lloyd, J., Bond, F. W., & Flaxman, P. E. (2013). The value of psychological flexibility: Examining psychological mechanisms underpinning a cognitive behavioral therapy intervention for burnout. Work & Stress, 27(2), 181–199. https://doi.org/10.1080/02678373.2013.782157
- Luoma, J. B., Hayes, S. C., & Walser, R. D. (2007). Learning ACT: An acceptance and commitment therapy skills-training manual for therapists. New Harbinger Publications.
- Luoma, J. B., Kohlenberg, B. S., Hayes, S. C., Bunting, K., & Rye, A. K. (2008). Reducing self-stigma in substance abuse through acceptance and commitment therapy: Model, manual development, and pilot outcomes. Addiction Research & Theory, 16(2), 149–165. https://doi.org/10.1080/16066350701850295
- Luciano, C., Valdivia-Salas, S., & Ruiz, F. J. (2004). The self as the context for rule-governed behavior. In S. C. Hayes, V. M. Follette, & M. M. Linehan (Eds.), Mindfulness and acceptance: Expanding the cognitive-behavioral tradition (pp. 63–94). Guilford Press.
- Masuda, A., Hayes, S. C., Sackett, C. F., & Twohig, M. P. (2004). 1 Cognitive defusion and self-relevant negative thoughts: Examining the impact of a ninety year old technique. Behaviour Research and Therapy, 42(4), 477–485. https://doi.org/10.1016/j.brat.2003.10.008
- Masuda, A., Levin, M. E., & Petersen, J. M. (2023). Cultural Adaptations of Acceptance and Commitment Therapy. In M. P. Twohig, M. E. Levin, & J. M. Petersen (Eds.), The Oxford Handbook of Acceptance and Commitment Therapy (online ed.). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780197550076.013.30
- McCracken, L. M. (2020). Psychological flexibility in chronic pain: Exploring the relevance of a process-based model for treatment development. In S. C. Hayes & S. G. Hofmann (Eds.), Beyond the DSM: Toward a process-based alternative for diagnosis and mental health treatment (pp. 199–223). Context Press/New Harbinger Publications.
- McLoughlin, S., & Roche, B. T. (2023). ACT: A Process-Based Therapy in Search of a Process. Behavior Therapy, 54(6), 939-955. https://doi.org/10.1016/j.beth.2022.07.010
- Meyer, E. C., Walser, R., Hermann, B., La Bash, H., DeBeer, B. B., Morissette, S. B., Kimbrel, N. A., Kwok, O. M., Batten, S. V., & Schnurr, P. P. (2018). Acceptance and Commitment Therapy for Co-Occurring Posttraumatic Stress Disorder and Alcohol Use Disorders in Veterans: Pilot Treatment Outcomes. Journal of Traumatic Stress, 31(5), 781–789. https://doi.org/10.1002/jts.22322
- NEFF, K. D. (2003). The Development and Validation of a Scale to Measure Self-Compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027
- Neff, K. D., & Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology, 69(1), 28–44. https://doi.org/10.1002/jclp.21923
- Öst, L. G. (2014). The efficacy of Acceptance and Commitment Therapy: An updated systematic review and meta-analysis. Behaviour Research and Therapy, 61, 105–121. https://doi.org/10.1016/j.brat.2014.07.018
- Pearson, A. N., Follette, V. M., & Hayes, S. C. (2012). Mindfulness and acceptance in treating disordered eating. In S. C. Hayes & S. M. Ciarrochi (Eds.), The Wiley Handbook of Contextual Behavioral Science (pp. 367–382). Wiley..
- Ruiz, F. J. (2010). A review of Acceptance and Commitment Therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. International Journal of Psychology & Psychological Therapy, 10(1), 125–162.
- Shapiro, S. L., Carlson, L. E., Astin, J. A., & Freedman, B. (2006). Mechanisms of mindfulness. Journal of Clinical Psychology, 62(3), 373–386. https://doi.org/10.1002/jclp.20237
- Spijkerman, M. P., Pots, W. T., & Bohlmeijer, E. T. (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 45, 102–114. https://doi.org/10.1016/j.cpr.2016.03.009
- Tang, Y.-Y., Ma, Y., Wang, J., Fan, Y., Feng, S., Lu, Q., … & Posner, M. I. (2007). Short-term meditation training improves attention and self-regulation. Proceedings of the National Academy of Sciences, 104(43), 17152–17156. https://doi.org/10.1073/pnas.0707678104
- Twohig, M. P., Hayes, S. C., & Masuda, A. (2006). Increasing willingness to experience obsessions: Acceptance and Commitment Therapy as a treatment for obsessive-compulsive disorder. Behavior Therapy, 37(1), 3–13. https://doi.org/10.1016/j.beth.2005.02.001
- Tyndall, I., Waldeck, D., Pancani, L., Whelan, R., Roche, B., & Dawson, D. L. (2019). The Acceptance and Action Questionnaire-II (AAQ-II) as a measure of experiential avoidance: Concerns over discriminant validity. Journal of Contextual Behavioral Science, 12, 278–284. https://doi.org/10.1016/j.jcbs.2018.09.005
- Vowles, K. E., & Thompson, M. (2011). Acceptance and commitment therapy for chronic pain. In L. M. McCracken (Ed.), Mindfulness and acceptance in behavioral medicine: Current theory and practice (pp. 31–60). New Harbinger Publications, Inc..
- Walser, R. D., & Westrup, D. (2007). Acceptance & commitment therapy for the treatment of post-traumatic stress disorder and trauma-related problems: A practitioner’s guide to using mindfulness and acceptance strategies. New Harbinger Publications.

Library Lecturer at Nurul Amin Degree College