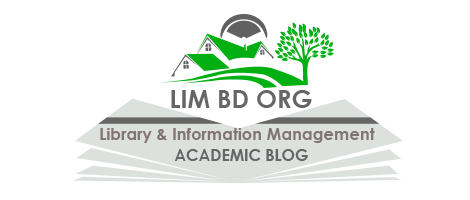
Components of the Biopsychosocial Model:
The biopsychosocial model is a holistic approach to understanding and explaining health and illness. It considers the interplay of biological, psychological, and social factors in influencing human health and well-being. Developed by psychiatrist George Engel in the 1970s, this model challenges the traditional biomedical model that focuses solely on biological factors. The biopsychosocial model recognizes the complex and dynamic nature of health, acknowledging that a variety of factors contribute to an individual’s overall well-being. In this article, we will explore some of essential components of the biopsychosocial model.
1. Biological Component:
The biological component of the biopsychosocial model delves into the physiological and genetic aspects of an individual’s health. It emphasizes the role of biological factors in shaping susceptibility to diseases, determining the body’s responses, and influencing overall well-being. Understanding this component is crucial for comprehending the foundation upon which health and illness are built.
1.1 Genetics: Genetics plays a pivotal role in shaping an individual’s health profile. Genes inherited from parents contribute to the predisposition for certain diseases or conditions. For example, if there is a family history of cardiovascular diseases, an individual may have a higher likelihood of developing similar issues. The study of genomics has provided insights into how specific genetic markers can influence disease risk, response to treatments, and even susceptibility to adverse drug reactions.
Example (Breast Cancer and BRCA Genes): Certain mutations in the BRCA1 and BRCA2 genes are associated with an increased risk of developing breast and ovarian cancers. Individuals with these mutations have a higher likelihood of developing these cancers compared to those without the mutations.
1.2 Neurochemical Processes: The intricate balance of neurotransmitters and their functions within the nervous system is a critical aspect of the biological component. Neurochemical processes influence mood, behavior, and cognitive functions, impacting mental health and well-being. Imbalances in neurotransmitters can contribute to the development of mental health disorders.
Example (Serotonin and Depression): Low levels of serotonin, a neurotransmitter that regulates mood, have been linked to depression. Antidepressant medications often work by increasing the availability of serotonin in the brain, helping to alleviate depressive symptoms.
1.3 Physiological Functions: The normal functioning of bodily systems, organs, and tissues is fundamental to overall health. Disruptions in physiological processes can lead to various health conditions and diseases. Understanding the biological underpinnings of illnesses is essential for effective diagnosis and treatment.
Example (Type 2 Diabetes and Insulin Resistance): In type 2 diabetes, the body becomes resistant to the effects of insulin, a hormone that regulates blood sugar. This physiological dysfunction results in elevated blood glucose levels, leading to diabetes. Lifestyle interventions and medications aim to address this underlying physiological issue.
2. Psychological Component:
The psychological component of the biopsychosocial model focuses on the influence of mental and emotional factors on an individual’s health. It recognizes the intricate connection between the mind and the body, emphasizing how thoughts, emotions, behaviors, and cognitive processes contribute to overall well-being. Understanding the psychological dimension is crucial for developing comprehensive interventions that address both mental and physical aspects of health.
2.1 Stress: Stress is a significant psychological factor that can have profound effects on health. Chronic stress, in particular, has been linked to a range of physical and mental health issues. Stress activates the body’s “fight or flight” response, releasing stress hormones such as cortisol, which, when prolonged, can contribute to various health problems.
Example (Cardiovascular Health): Chronic stress is associated with an increased risk of cardiovascular diseases. The constant release of stress hormones can lead to elevated blood pressure, inflammation, and changes in heart rate, all of which contribute to the development and progression of heart conditions.
2.2 Mental Health Disorders: Mental health conditions, such as anxiety and depression, are integral components of the psychological aspect of the biopsychosocial model. These conditions not only impact mental well-being but also have tangible effects on physical health, affecting behaviors, cognition, and overall functioning.
Example (Depression and Physical Health): Individuals with depression often experience physical symptoms such as changes in appetite, sleep disturbances, and fatigue. Moreover, depression has been linked to a higher risk of developing chronic conditions like diabetes and cardiovascular diseases.
2.3 Cognitive Processes: The way individuals perceive and interpret information, known as cognitive processes, plays a crucial role in shaping health behaviors. Attitudes, beliefs, and coping strategies influence decision-making related to lifestyle choices, adherence to medical advice, and overall health management.
Example (Health Beliefs and Lifestyle Choices): Someone with positive health beliefs may be more likely to engage in preventive health behaviors, such as regular exercise and a balanced diet. Conversely, negative health beliefs or misconceptions may contribute to unhealthy lifestyle choices.
3. Social Component:
The social component of the biopsychosocial model explores the impact of social, cultural, and environmental factors on an individual’s health. It emphasizes the role of social interactions, support systems, socioeconomic status, and cultural context in shaping health outcomes. Recognizing the influence of the social environment is essential for understanding health disparities and tailoring interventions to diverse populations.
3.1 Social Support: Social support refers to the network of relationships and assistance from family, friends, and community. The presence or absence of social support can significantly influence an individual’s ability to cope with stress, manage health conditions, and adopt healthy behaviors.
Example (Recovery from Illness): Studies have shown that individuals with strong social support networks tend to have better recovery outcomes after illness or surgery. Emotional and practical support from loved ones can positively impact the healing process.
3.2 Socioeconomic Status: Socioeconomic status (SES) encompasses factors such as income, education, and occupation. It plays a crucial role in determining access to resources, healthcare services, and opportunities for a healthy lifestyle. Disparities in SES contribute to health inequalities.
Example (Access to Healthcare): Individuals with higher socioeconomic status often have better access to healthcare resources, including preventive services and timely medical interventions. Lower SES is associated with barriers to healthcare, leading to delayed diagnoses and poorer health outcomes.
3.3 Cultural Influences: Cultural norms, values, and beliefs shape health behaviors and influence how individuals perceive and manage their well-being. Considering cultural diversity is essential for tailoring healthcare approaches that respect and align with the cultural context of the individual or community.
Example (Health Practices): Cultural influences can impact health practices, such as dietary choices and traditional healing methods. For instance, cultural dietary preferences may influence an individual’s nutritional intake and, consequently, their health outcomes.
4. Interactions and Integration:
The strength of the biopsychosocial model lies in recognizing that the biological, psychological, and social components are not isolated entities but are interconnected and interactive. Understanding how these factors influence each other is essential for comprehending the complexity of health and illness. The interactions and integration of these components provide a more nuanced understanding of the holistic nature of human well-being.
4.1 Chronic Pain as an Example: Consider chronic pain, a complex health issue that can be effectively analyzed through the lens of the biopsychosocial model. The biological component involves identifying the physiological source of pain, such as a musculoskeletal injury. However, the psychological aspect recognizes that the perception of pain is influenced by emotional factors, like anxiety and depression. Social factors, such as the availability of social support or a stressful work environment, can further impact an individual’s ability to cope with and manage pain.
Example (Biological): A person may have a herniated disc causing chronic back pain. (Psychological): Anxiety and depression can amplify the perception of pain and hinder the coping mechanisms. (Social): Lack of social support or a stressful work environment may contribute to the persistence of pain.
4.2 Holistic Assessment: The biopsychosocial model emphasizes the importance of holistic assessments in healthcare. Instead of focusing solely on symptoms or biomarkers, healthcare professionals consider the broader context of an individual’s life, including their psychological state, social environment, and cultural background. This holistic approach allows for a more thorough understanding of the factors influencing health and guides personalized interventions.
Example (Holistic Mental Health Assessment): When evaluating a person’s mental health, healthcare professionals consider not only the symptoms but also factors such as life stressors, social support, and cultural influences. This comprehensive assessment informs treatment plans that address the individual’s unique needs.
4.3 Preventive Strategies: The biopsychosocial model has significant implications for preventive strategies. Rather than focusing solely on reducing biological risk factors, interventions can address psychological and social determinants of health. This approach acknowledges that preventing illness goes beyond medical interventions to include lifestyle modifications, stress management, and social support.
Example (Cardiovascular Disease Prevention): Instead of solely prescribing medications for hypertension, preventive strategies may involve lifestyle changes (exercise and diet), stress reduction techniques, and community programs promoting heart-healthy behaviors.
4.4 Comprehensive Treatment Approaches: When dealing with health conditions, the biopsychosocial model supports comprehensive treatment approaches that address all relevant components. Integrating biological, psychological, and social interventions can enhance the effectiveness of healthcare strategies and improve overall outcomes.
Example (Addiction Treatment): In addressing substance abuse, a comprehensive treatment plan may include medical detoxification (biological), counseling and therapy to address underlying psychological issues, and support groups or community involvement to foster social connections.
5. Preventive and Therapeutic Implications:
The biopsychosocial model has profound implications for both preventive measures and therapeutic interventions. It encourages a comprehensive approach that considers biological, psychological, and social factors, recognizing that addressing health from multiple dimensions is essential for promoting well-being and preventing illness.
5.1 Health Promotion: The biopsychosocial model shifts the focus from merely treating diseases to promoting overall health and well-being. Health promotion strategies aim to enhance the quality of life by addressing not only biological risk factors but also psychological and social determinants of health.
Example (Stress Management Programs): Implementing stress management programs in workplaces or communities can be a health promotion strategy. These programs may include mindfulness sessions, counseling, and education on coping strategies, addressing the psychological component of health.
5.2 Patient Education: Educating individuals about the interconnected nature of biological, psychological, and social factors empowers them to take a more active role in their health. Patient education can promote awareness of the importance of lifestyle choices, mental well-being, and social support in maintaining and improving health.
Example (Diabetes Education): For individuals with diabetes, education can go beyond medication management to include information on nutrition, exercise, and stress management. This holistic approach helps individuals better manage their condition and prevent complications.
5.3 Behavioral Interventions: Behavioral interventions target not only biological aspects but also psychological and social factors influencing health behaviors. These interventions aim to modify behaviors through strategies such as cognitive-behavioral therapy, motivational interviewing, and behavior change programs.
Example (Smoking Cessation Programs): Helping individuals quit smoking involves addressing both the physical addiction (biological) and the psychological aspects of smoking behavior. Behavioral interventions can provide support to manage cravings, address triggers, and explore healthier coping mechanisms.
5.4 Workplace Wellness Programs: Recognizing the impact of the social environment on health, workplace wellness programs have gained popularity. These programs often encompass physical health initiatives, mental health support, and social activities to create a holistic approach to employee well-being.
Example (Fitness Challenges): Workplace wellness programs may include fitness challenges to encourage physical activity (biological), workshops on stress management and resilience (psychological), and team-building activities to foster social connections among employees.
5.5 Community-Based Initiatives: Community-based interventions acknowledge the influence of social determinants on health. These initiatives aim to create supportive environments, strengthen social ties, and improve access to resources, contributing to the overall health and well-being of community members.
Example (Community Gardens): Establishing community gardens addresses both physical activity (biological) and social connections (social). Individuals engage in physical activity while cultivating social bonds through shared gardening activities.
5.6 Integrated Healthcare: Healthcare delivery systems can adopt an integrated care approach that considers the biopsychosocial context. Collaborative care models involve interdisciplinary teams working together to address biological, psychological, and social aspects of health, promoting better coordination and outcomes.
Example (Chronic Disease Management Clinics): Integrated clinics for managing chronic conditions may involve healthcare professionals from various fields, such as physicians, psychologists, and social workers. This collaborative approach ensures a comprehensive understanding and treatment of the patient’s health.
6. Patient-Centered Care:
One of the key tenets of the biopsychosocial model is the promotion of patient-centered care. This approach recognizes the individuality of each person and considers their unique biological, psychological, and social context. Patient-centered care involves collaboration between healthcare providers and patients to develop a personalized and holistic approach to diagnosis, treatment, and overall well-being.
6.1 Individualized Treatment Plans: Patient-centered care emphasizes the development of individualized treatment plans that consider not only the biological aspects of a condition but also the psychological and social factors influencing the patient’s health. This approach recognizes that what works for one person may not be suitable for another, and treatment plans need to be tailored to the individual’s needs and preferences.
Example (Cancer Treatment): In cancer care, a patient-centered approach involves considering the biological aspects of the cancer, the psychological impact of the diagnosis, and the patient’s social support network. Treatment plans may incorporate not only medical interventions but also psychological support services and assistance in coordinating social support.
6.2 Shared Decision-Making: Patient-centered care promotes shared decision-making, where healthcare providers and patients collaborate in making decisions about treatment options. This involves a transparent exchange of information, discussing the potential benefits and risks of different interventions, and considering the patient’s values and preferences.
Example (Treatment Options): When deciding on a course of treatment for a chronic condition like arthritis, a patient-centered approach involves discussing various treatment options, including medications, physical therapy, and lifestyle changes. The patient’s preferences and priorities are taken into account in developing a plan that aligns with their goals.
6.3 Emphasis on Communication: Effective communication is a cornerstone of patient-centered care. Healthcare providers need to engage in open and respectful communication, actively listening to patients’ concerns, and providing information in a way that is understandable. This ensures that patients feel heard and involved in their care.
Example (Mental Health Treatment): In mental health care, a patient-centered approach involves regular communication between the patient and mental health professionals. This includes discussing treatment options, understanding the patient’s experiences, and collaboratively adjusting treatment plans based on the patient’s feedback.
6.4 Incorporating Patient Values: Patient-centered care acknowledges the importance of considering the patient’s values, beliefs, and cultural background in the healthcare process. Understanding and incorporating these aspects into the treatment plan can enhance the effectiveness of interventions and improve patient satisfaction.
Example (End-of-Life Care): In end-of-life care, a patient-centered approach involves discussing the patient’s values and preferences regarding interventions, hospice care, and the overall approach to the end-of-life process. This ensures that the care provided aligns with the patient’s wishes.
6.5 Holistic Well-Being: Beyond addressing specific health conditions, patient-centered care recognizes the importance of promoting overall well-being. This involves considering the patient’s lifestyle, social relationships, and mental health in the context of their healthcare plan.
Example (Preventive Care): A patient-centered approach to preventive care involves discussing not only routine screenings and vaccinations but also addressing lifestyle factors, stressors, and social determinants that may impact the patient’s health in the long term.
6.6 Continuity of Care: Patient-centered care promotes continuity and coordination in healthcare. This involves ensuring that patients receive consistent and coherent care across different healthcare providers and settings. Effective collaboration and communication among healthcare professionals contribute to a seamless and patient-centered healthcare experience.
Example (Chronic Disease Management): For individuals with chronic conditions, such as diabetes, a patient-centered approach involves coordinating care between primary care physicians, specialists, and allied health professionals. This ensures that the patient receives comprehensive and well-coordinated care for their ongoing health needs.
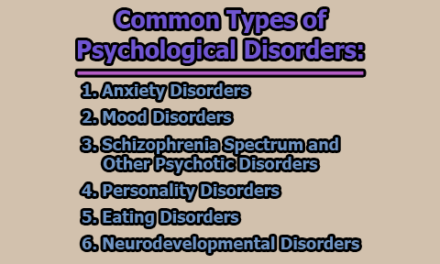
7. Critiques and Challenges:
While the biopsychosocial model offers a holistic and comprehensive framework for understanding health and illness, it is not without its critiques and challenges. Examining these criticisms helps in understanding the limitations and potential areas for improvement in the application of the model.
7.1 Lack of Clear Guidelines for Implementation: One of the primary criticisms of the biopsychosocial model is the lack of clear guidelines for implementation. Critics argue that the model, while conceptually appealing, can be challenging to apply consistently in clinical practice. The absence of standardized protocols makes it difficult for healthcare professionals to systematically integrate the biological, psychological, and social aspects in their assessments and treatments.
Example (Diagnostic Criteria): In contrast to the biomedical model, which often relies on standardized diagnostic criteria and treatment algorithms, the biopsychosocial model provides a broad framework without specifying clear procedures for incorporating each component.
7.2 Difficulty in Isolating and Measuring Components: Another critique relates to the challenge of isolating and measuring each component independently. While the model emphasizes the interconnectedness of biological, psychological, and social factors, research methodologies often struggle to separate and quantify these elements accurately. This limitation can hinder the development of empirical evidence and may make it challenging to draw clear conclusions about the model’s effectiveness.
Example (Research Studies): Research attempting to measure the impact of psychological and social factors on health outcomes often faces methodological challenges. For instance, isolating the specific influence of social support on recovery from illness may be complicated by confounding variables.
7.3 Subjectivity of Psychological and Social Factors: The subjective nature of psychological and social factors poses another challenge. While biological markers can be objectively measured, psychological and social variables are often based on self-reporting and individual interpretations. This subjectivity can introduce bias and make it difficult to establish standardized assessments.
Example (Assessment of Stress): Assessing stress levels relies heavily on self-reporting, which can be influenced by individual perceptions and cultural factors. This subjectivity may limit the reliability and generalizability of stress-related research findings.
7.4 Complexity and Time Constraints in Clinical Settings: The biopsychosocial model’s emphasis on considering multiple dimensions of health adds complexity to clinical assessments and interventions. In busy healthcare settings, where time constraints are common, healthcare professionals may find it challenging to conduct comprehensive assessments that address biological, psychological, and social aspects adequately.
Example (Primary Care Visits): In primary care settings, physicians may have limited time for patient visits. Balancing the need for addressing immediate health concerns with a comprehensive exploration of psychological and social factors can be logistically challenging.
7.5 Integration in Medical Education: The biopsychosocial model’s integration into medical education has been uneven, with some critics arguing that the model’s principles are not consistently emphasized in curricula. The traditional focus on biomedical aspects in medical training may result in healthcare professionals who are less adept at applying the biopsychosocial approach in their practice.
Example (Training Programs): Some medical schools and training programs may still predominantly emphasize the biomedical model, potentially leading to a gap in healthcare professionals’ ability to apply the biopsychosocial model effectively in real-world scenarios.
8. Research and Advancements:
The biopsychosocial model has spurred significant research and advancements across various disciplines, including medicine, psychology, sociology, and public health. Researchers continue to explore the complex interactions between biological, psychological, and social factors to deepen our understanding of health and inform more effective interventions. The model’s influence has extended beyond theoretical frameworks, driving empirical investigations and innovative approaches to healthcare.
8.1 Mind-Body Connections: Advances in research have illuminated the intricate connections between the mind and the body, validating the importance of psychological factors in influencing physical health. Psychoneuroimmunology, for instance, explores how psychological states impact the immune system, providing insights into the role of emotions, stress, and mental health in overall well-being.
Example (Mindfulness and Health): Research on mindfulness meditation has demonstrated its positive effects on mental health and, subsequently, its potential to influence physical health. Mindfulness practices have been associated with reduced stress, improved immune function, and better overall health outcomes.
8.2 Epigenetics and Gene-Environment Interactions: The exploration of epigenetics has shed light on how environmental factors, including psychological and social influences, can impact gene expression. Understanding gene-environment interactions has significant implications for personalized medicine and interventions that consider an individual’s unique genetic and environmental makeup.
Example (Childhood Adversity and Gene Expression): Research has shown that early-life adversity can influence gene expression patterns. Adverse experiences, such as trauma or neglect, may alter gene regulation, affecting stress response systems and susceptibility to certain health conditions later in life.
8.3 Biopsychosocial Approaches in Mental Health: Advancements in mental health research have embraced biopsychosocial approaches, recognizing the multifaceted nature of mental disorders. Integrative treatments that combine pharmacotherapy with psychotherapy, lifestyle interventions, and social support have gained prominence, reflecting a holistic understanding of mental health.
Example (Comprehensive Treatment for Depression): Research supports the effectiveness of combining antidepressant medications with cognitive-behavioral therapy (CBT) and lifestyle modifications in treating depression. This approach acknowledges the biological, psychological, and social dimensions of mental health.
8.4 Social Determinants of Health: Research on social determinants of health has expanded, investigating how social, economic, and environmental factors contribute to health disparities. This body of research informs public health interventions aimed at addressing social inequalities and improving overall population health.
Example (Housing and Health): Studies have explored the impact of housing conditions on health outcomes. Individuals living in inadequate housing may face increased risks of respiratory problems, mental health issues, and other health challenges, highlighting the importance of addressing social determinants.
8.5 Integration of Technology: Advances in technology have facilitated the integration of the biopsychosocial model into healthcare delivery. Digital health interventions, mobile applications, and telemedicine platforms are being designed to address not only biological aspects but also psychological and social factors, enhancing accessibility and personalization of healthcare.
Example (Telepsychiatry): The use of telepsychiatry allows individuals to access mental health services remotely. This technology-driven approach enables the integration of psychological support with biological treatments, expanding mental health care accessibility.
8.6 Preventive Medicine and Lifestyle Interventions: Research on preventive medicine and lifestyle interventions has grown, emphasizing the role of behavior and environmental factors in health promotion. Studies exploring the impact of diet, physical activity, and stress management on overall well-being contribute to the development of evidence-based guidelines for preventive healthcare.
Example (Cardiometabolic Health): Research on lifestyle interventions, such as the Mediterranean diet and regular exercise, has shown significant benefits for cardiometabolic health. These findings underscore the importance of addressing both biological and behavioral factors in preventing cardiovascular diseases.
8.7 Biopsychosocial Models in Chronic Disease Management: The development of biopsychosocial models tailored to specific chronic conditions has become a focus of research. Chronic disease management programs that integrate biological, psychological, and social elements aim to enhance patient outcomes and quality of life.
Example (Integrated Care for Diabetes): Research explores integrated care models for diabetes management, incorporating medical treatment, psychological support, and lifestyle interventions. These holistic approaches aim to improve glycemic control and reduce the impact of diabetes on overall health.
In conclusion, the biopsychosocial model provides a comprehensive framework for understanding health and illness by incorporating biological, psychological, and social factors. It emphasizes the dynamic interactions between these components and recognizes the importance of considering the individual within their broader context. This holistic approach has implications for preventive measures, therapeutic interventions, and patient-centered care, contributing to a more nuanced and effective understanding of health in diverse populations.
References:
- Cozolino, L. (2017). The neuroscience of psychotherapy: Healing the social brain. Norton and Company.
- Engel, D. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196, 129–136.
- Garcia-Gomez, P., Van Kippersluis, O., O’Donnell, E., & Van Doorslaer, H. (2013). Long term and spillover effects of health shocks on employment and income. Journal of Human Resources, 48(4), 873–909.
- Lehman, B., David, D., & Gruber, J. (2017). Rethinking the biopsychosocial model of health: Understanding health as a dynamic system. Social and Personality Psychology Compass, 11(8), 123–128.
- Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The relationship between physical and mental health: A mediation analysis. Journal of Social Science in Medicine, 195, 24–49.
- Papadimitriou, C. (2017). The biopsychosocial model: 40 years of application in psychiatry. Psychiatry, 28, 107–120.
- Sharma, V., Trakoo, M., Subramaniam, V., Rajajeyakumar, M., Bhavanani, A., & Sahai, A. (2013). Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. International Journal of Yoga, 6(2), 104–110.
- Steptoe, A., Shanker, A., Demakakos, P., & Wardle, J. (2012). Social isolation, loneliness and all-cause mortality in older men and women. National Academy of Science, 111(15), 5797–5811.
- Tripathi, A., Das, A., & Kar, S. (2019). Biopsychosocial model in contemporary psychiatry: Current validity and future prospects. Indian Journal of Psychological Medicine, 41(6), 582–585.
- Wade, D., & Halligan, P. (2017). The biopsychosocial model of illness: A model whose time has come. Clinical Rehabilitation, 31(8), 995–1004.

Former Student at Rajshahi University