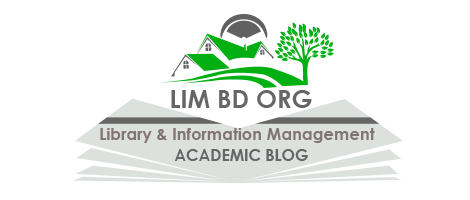
The Role of Behavioral Extinction in Clinical Psychology:
Behavioral extinction is a psychological intervention that aims to reduce or eliminate maladaptive responses by gradually decreasing reinforcement. In clinical contexts, extinction plays a crucial role in therapeutic interventions, particularly for individuals experiencing fear, anxiety, or maladaptive behaviors. It involves “deliberate, planned, and repeated exposure to what is feared, including objects, situations, memories, images, and body sensations” (Smits et al., 2022, p. 203). By exposing individuals to feared stimuli without the expected negative consequences, extinction helps break the cycle of conditioned fear responses. This article explores the role of behavioral extinction in clinical psychology which helps to treat various psychological and physiological conditions, including asthma-related anxiety, pregnancy-related stress, childhood anxiety, and eating disorders, as well as its role in obsessive-compulsive disorder (OCD), phobias, post-traumatic stress disorder (PTSD), social anxiety disorder, panic disorder, and generalized anxiety disorder (GAD).
1. Asthma-Related Anxiety: Asthma is not only a physiological condition but also a significant source of psychological distress. Many individuals with asthma experience panic, generalized anxiety, and health-related anxiety due to the fear of asthma attacks. The psychological burden can worsen symptoms and lead to avoidance behaviors, such as avoiding exercise or social situations that might trigger an attack.
Behavioral extinction, particularly when integrated with cognitive behavioral therapy (CBT) and exposure therapy, helps asthma patients dissociate their fear from the physical symptoms of their condition. One approach involves gradual exposure to breathlessness-inducing exercises, such as controlled physical activity, allowing patients to experience breathlessness in a safe environment. This method reduces anxiety associated with mild respiratory distress and prevents excessive panic responses. Additionally, children with asthma benefit from structured coping mechanisms that help them manage triggers more effectively. By integrating behavioral extinction techniques, therapists can reduce the emotional distress linked to asthma and improve overall health outcomes.
2. Pregnancy-Related Anxiety: Pregnancy, particularly the prospect of labor and delivery, can be an overwhelming experience for many women. Research indicates that approximately 15% of pregnant women suffer from anxiety disorders, yet access to appropriate treatment remains limited (Smits et al., 2022). The anticipation of childbirth can cause excessive worry, leading to heightened stress levels that negatively impact both the mother and the developing fetus.
Therapeutic interventions using behavioral extinction techniques have demonstrated effectiveness in managing prenatal anxiety. CBT, combined with extinction-based exposure techniques, helps reduce stress by exposing pregnant women to anxiety-inducing thoughts and scenarios in a controlled manner. For example, structured therapy sessions may involve discussing fears related to childbirth while implementing relaxation strategies, gradually reducing the distress associated with these thoughts. Additionally, group therapy can provide social support, though it must be carefully managed to prevent exacerbation of social anxiety in some individuals. With the rise of digital health interventions, online therapy has emerged as a promising alternative, increasing accessibility while lowering costs. However, further research is required to assess the long-term effectiveness of digital interventions for pregnancy-related anxiety.
3. Anxiety in Children: Childhood anxiety can stem from various sources, including genetic predisposition, environmental influences, and insecure attachment to caregivers. Many children struggle with low self-efficacy, which can manifest in excessive fears and avoidance behaviors. Anxiety disorders in children can lead to difficulties in academic performance, social interactions, and emotional development.
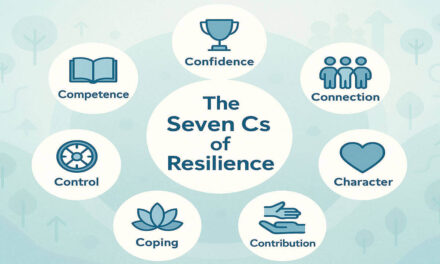
Behavioral extinction techniques, particularly exposure therapy, have been extensively used to help children confront and overcome their fears. In structured therapeutic settings, children are gradually and systematically exposed to anxiety-provoking stimuli, such as feared objects, social situations, or separation scenarios, in a safe and controlled environment. This process allows children to unlearn their fear responses over time. Additionally, therapy sessions are tailored to the individual child, taking into account their family dynamics, school environment, and unique triggers. By using behavioral extinction strategies, therapists help children develop resilience and reduce avoidance behaviors, ultimately improving their ability to cope with everyday challenges.
4. Eating Disorders and Behavioral Extinction: Eating disorders, such as anorexia nervosa, bulimia nervosa, and binge-eating disorder, are complex conditions involving both psychological and physiological factors. These disorders are often reinforced by maladaptive behaviors, such as food restriction, purging, and avoidance of specific food groups. Behavioral extinction techniques, particularly exposure therapy, have been effective in treating eating disorders by helping individuals confront and reduce their fear-based responses to food and eating.
One common approach involves exposure to feared foods, where patients are gradually introduced to food items they avoid due to irrational fears of weight gain or negative physical reactions. In a controlled therapeutic setting, patients learn to sit with the discomfort and anxiety that arises, allowing their conditioned fear responses to decrease over time. Additionally, cognitive restructuring techniques help patients identify and challenge distorted beliefs about food, making extinction strategies more effective. Since eating disorders are often influenced by environmental and social factors, treatment plans incorporating family support and structured reinforcement systems significantly improve outcomes.
5. Obsessive-Compulsive Disorder (OCD): Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts (obsessions) and repetitive behaviors (compulsions) that individuals engage in to reduce anxiety. These compulsions are maintained through negative reinforcement—performing the compulsive act temporarily relieves distress, reinforcing the cycle. Behavioral extinction plays a central role in exposure and response prevention (ERP), the most effective treatment for OCD.
ERP involves systematically exposing patients to their obsessive fears while preventing the corresponding compulsive behaviors. For example, a person with contamination-related OCD may be exposed to a perceived unclean surface but instructed not to engage in excessive handwashing. Over time, as the patient learns that their anxiety naturally subsides without engaging in the compulsion, the conditioned fear response weakens. Research has consistently shown that ERP leads to significant reductions in OCD symptoms, improving patients’ ability to function in daily life. However, successful extinction requires sustained practice and professional guidance, as avoidance behaviors can easily re-emerge without proper reinforcement.
6. Phobias and Behavioral Extinction: Phobias are intense, irrational fears of specific objects or situations, such as heights, enclosed spaces, or spiders. These fears can severely impact an individual’s ability to function in everyday life. Behavioral extinction is a key component of graded exposure therapy, which gradually exposes individuals to their feared stimuli in a controlled and systematic manner.
For instance, a person with a fear of flying may begin by viewing images of airplanes, followed by visiting an airport, sitting in a stationary plane, and eventually taking a short flight. Each step is designed to reduce fear and anxiety through repeated exposure without reinforcement of avoidance behaviors. Over time, the fear response diminishes as the brain learns that the feared stimulus does not lead to catastrophic outcomes. Graded exposure has proven to be highly effective in treating specific phobias, often leading to long-term improvements in anxiety management. However, treatment must be tailored to the individual’s tolerance level, as excessive exposure too soon can lead to heightened distress rather than extinction.
7. Post-Traumatic Stress Disorder (PTSD): PTSD develops following exposure to traumatic events and is often associated with intense fear and avoidance behaviors. Extinction therapy, particularly prolonged exposure therapy, helps individuals process traumatic memories without reinforcing fear responses. Patients repeatedly recall their trauma in a safe setting until their distress levels decrease, enabling them to regain control over their emotional responses.
For example, a veteran with combat-related PTSD might gradually revisit distressing memories through guided therapy sessions. Over time, this reduces the overwhelming emotional reactions associated with these memories. The therapy also includes real-world exposure, such as visiting crowded places if avoidance behaviors have developed due to past trauma. By reducing avoidance behaviors and breaking the fear association, extinction therapy improves PTSD outcomes.
8. Social Anxiety Disorder: Social anxiety disorder involves excessive fear of social interactions, often leading to avoidance of social situations. Behavioral extinction techniques, particularly exposure therapy, help individuals gradually confront feared social scenarios.
For example, a person who fears public speaking might start by practicing speeches alone, then progress to speaking in front of a small group, and ultimately present to a larger audience. Each exposure session helps reduce anxiety, enabling individuals to develop confidence in social interactions. Behavioral extinction therapy for social anxiety often includes cognitive restructuring, where individuals learn to reframe negative self-perceptions, making social engagements less intimidating over time.
9. Panic Disorder: Panic disorder is characterized by sudden and intense episodes of fear, often accompanied by physical symptoms such as heart palpitations and dizziness. Behavioral extinction techniques focus on interoceptive exposure, where patients are gradually exposed to bodily sensations associated with panic attacks.
For instance, a person who fears dizziness might engage in controlled spinning exercises to simulate the sensation in a safe environment. Over time, they learn that these sensations are not dangerous, reducing their fear response. This approach helps break the association between physical sensations and catastrophic thinking, allowing individuals to regain control over their panic symptoms.
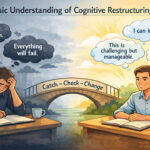
10. Generalized Anxiety Disorder (GAD): Generalized anxiety disorder (GAD) involves chronic and excessive worry about everyday situations. Unlike phobias or PTSD, where anxiety is linked to specific triggers, GAD is characterized by persistent, diffuse worry. Behavioral extinction techniques help individuals break the cycle of excessive worrying by exposing them to uncertainty and reducing avoidance behaviors.
For example, a person with GAD who excessively checks the news for reassurance might be encouraged to gradually reduce their checking behavior. Over time, they learn that uncertainty does not necessarily lead to catastrophic outcomes, helping them tolerate distress more effectively. Behavioral extinction, often combined with mindfulness techniques, helps individuals shift their focus away from anxiety-driven thoughts and toward present-moment awareness, leading to significant reductions in worry and stress.
It is apparent that behavioral extinction is a powerful tool in clinical psychology, helping individuals unlearn maladaptive responses and develop healthier coping mechanisms. From reducing asthma-related anxiety to addressing pregnancy stress, childhood anxiety, and eating disorders, extinction-based therapies offer effective solutions for various psychological challenges. Additionally, extinction techniques play a significant role in treating OCD, phobias, PTSD, social anxiety disorder, panic disorder, and GAD, providing individuals with long-term relief from debilitating fears and compulsions. While these interventions have proven successful, their effectiveness depends on careful implementation, individualization, and continued research. As psychological science evolves, refining extinction-based therapies will be essential in providing more accessible and impactful mental health treatments.
Frequently Asked Questions (FAQs):
What is behavioral extinction in psychology?
Behavioral extinction is a psychological process that involves reducing or eliminating learned behaviors by removing the reinforcement that maintains them. It is widely used in clinical settings to help individuals overcome maladaptive behaviors, fears, and anxieties.
How does extinction differ from punishment?
Extinction involves the gradual weakening of a behavior by withholding reinforcement, whereas punishment introduces an aversive stimulus to decrease behavior. Unlike punishment, extinction is generally considered a more ethical and sustainable approach in therapy.
What are some common applications of extinction in therapy?
Extinction-based therapies are used in treating conditions such as obsessive-compulsive disorder (OCD), phobias, post-traumatic stress disorder (PTSD), social anxiety disorder, and eating disorders. It is often combined with exposure therapy and cognitive behavioral therapy (CBT).
Can extinction therapy work for all individuals?
While extinction therapy is highly effective, individual differences such as personality, severity of the condition, and previous treatment history can influence outcomes. In some cases, additional therapeutic interventions may be required.
What challenges are associated with extinction-based therapy?
Challenges include spontaneous recovery (return of behavior after a period of extinction), renewal effect (behavior reappearing in different contexts), and resistance to extinction due to strong reinforcement histories.
Is exposure therapy the same as extinction?
Exposure therapy is a technique that utilizes extinction principles by exposing individuals to feared stimuli without reinforcement. While exposure therapy is one method of extinction, extinction can also be achieved in other ways, such as removing attention from undesired behaviors.
How long does it take for behavioral extinction to be effective?
The duration varies depending on factors such as the complexity of the behavior, frequency of reinforcement, and individual response. Some individuals show progress within weeks, while others may require long-term therapy.
Can extinction therapy be used for addiction treatment?
Yes, extinction is applied in addiction treatment through cue-exposure therapy, where individuals are repeatedly exposed to drug-related cues without reinforcement, weakening the craving response.
What are alternative treatments if extinction does not work?
If extinction alone is insufficient, clinicians may incorporate cognitive restructuring, pharmacotherapy, mindfulness techniques, or other behavioral interventions to enhance treatment effectiveness.
Is extinction therapy suitable for children?
Yes, extinction techniques are often used in treating childhood anxiety, phobias, and behavioral disorders. However, therapy must be adapted to the child’s developmental level and individual needs to ensure effectiveness.
References:
- Abramowitz, J. S. (2013). The practice of exposure therapy: Relevance of cognitive-behavioral theory and extinction theory. Behavior Therapy, 44(4), 548–558. https://doi.org/10.1016/j.beth.2013.03.003
- DeAngelis, T. (2019). Better relationships with patients lead to better outcomes. Monitor on Psychology, 50(10). https://www.apa.org/monitor/2019/11/ce-corner-relationships
- Smits, J. A. J., Jacquart, J., Abramowitz, J., Arch, J., & Margraf, J. (2022). Clinical guide to exposure therapy: Beyond phobias. Springer International Publishing Springer.

Library Lecturer at Nurul Amin Degree College