The Role of Exercise in Controlling Blood Sugar Levels:
Diabetes mellitus, commonly known as diabetes, is a chronic medical condition characterized by elevated blood sugar levels. It affects millions of people worldwide and is associated with numerous health complications. Managing blood sugar levels is paramount in diabetes management, and exercise plays a crucial role in achieving this goal. In this article, we will explore the role of exercise in controlling blood sugar levels.
Understanding Blood Sugar and Diabetes:
To comprehend the significance of exercise in managing blood sugar levels, it is imperative to first establish a fundamental understanding of blood sugar regulation and the two primary forms of diabetes: Type 1 and Type 2.
Blood Sugar Regulation: Glucose, derived from the carbohydrates we consume, serves as the primary source of energy for our body’s cells. When we eat, our digestive system breaks down carbohydrates into glucose molecules. These glucose molecules then enter the bloodstream, leading to an increase in blood sugar levels.
However, for glucose to be utilized by the body’s cells and tissues as an energy source, it requires a hormone called insulin. Insulin is produced by specialized cells in the pancreas known as beta cells. Insulin acts as a key, facilitating the entry of glucose into cells, thus lowering blood sugar levels.
In individuals with diabetes, the normal blood sugar regulation process is disrupted:
- Type 1 Diabetes: In Type 1 diabetes, the immune system mistakenly attacks and destroys the beta cells in the pancreas. Consequently, the body produces little to no insulin, leading to high blood sugar levels. This form of diabetes typically develops early in life and requires lifelong insulin therapy.
- Type 2 Diabetes: Type 2 diabetes is characterized by a combination of insulin resistance and impaired insulin secretion. Initially, the body’s cells do not respond effectively to insulin, leading to elevated blood sugar levels. Over time, the pancreas may also produce insufficient insulin. Type 2 diabetes is often associated with lifestyle factors such as obesity, physical inactivity, and poor diet.
The Connection Between Exercise and Blood Sugar:
Exercise is a powerful and versatile tool for effectively managing blood sugar levels, irrespective of whether an individual has Type 1 or Type 2 diabetes. Physical activity induces a series of essential physiological changes in the body that play a pivotal role in the regulation of blood sugar. These changes include increased insulin sensitivity, enhanced glucose uptake by muscles, activation of glucose transporters, regulation of liver glucose output, and the facilitation of weight management.
1. Increased Insulin Sensitivity: Exercise has a profound impact on the body’s sensitivity to insulin. Insulin sensitivity refers to the ability of cells to efficiently respond to insulin signals and take up glucose from the bloodstream. When we engage in regular exercise, especially aerobic and resistance training, the body becomes more sensitive to insulin. This heightened sensitivity means that even individuals with insulin resistance, a hallmark of Type 2 diabetes, can benefit from exercise by improving their ability to use insulin effectively. This effect is well-documented in scientific literature (DeFronzo et al., 2015).
2. Muscle Contraction: During exercise, muscles contract and demand more energy to support the increased activity. To meet this demand, muscles actively absorb glucose directly from the bloodstream, bypassing the need for insulin. This direct uptake of glucose by muscle cells effectively lowers blood sugar levels during and after physical activity. Muscle contraction-induced glucose uptake is a significant mechanism underlying the blood sugar-lowering effect of exercise (Hawley et al., 2014).
3. Glucose Transporter Activation: Exercise stimulates the activation of glucose transporters, primarily GLUT4, on the cell membranes of muscle cells. These transporters act as “gatekeepers” that facilitate the entry of glucose into the cells. As a result of exercise, more GLUT4 transporters are translocated to the cell membrane, making it easier for glucose to enter muscle cells. This increased glucose uptake contributes to the regulation of blood sugar levels (Richter & Hargreaves, 2013).
4. Liver Glucose Output Regulation: The liver plays a crucial role in blood sugar regulation. It can release stored glucose into the bloodstream when needed for energy. During exercise, the body’s demand for glucose increases, and the liver’s glucose output is carefully regulated. Exercise helps control this release, preventing excessive production of glucose by the liver. This mechanism helps maintain stable blood sugar levels during physical activity (Perry et al., 2015).
5. Weight Management: Regular physical activity is instrumental in achieving and maintaining a healthy body weight. For individuals with Type 2 diabetes, weight management is a critical component of blood sugar control. Exercise helps burn calories, build lean muscle mass, and reduce body fat. By achieving and maintaining a healthy weight, individuals can significantly improve insulin sensitivity and enhance their overall blood sugar control (Rosenberg et al., 2007).
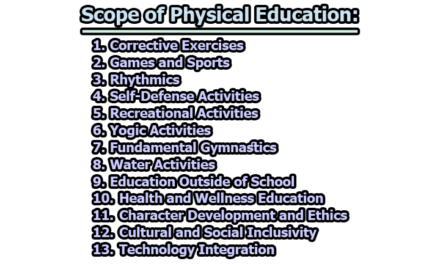
Types of Exercise for Blood Sugar Control:
Exercise is a versatile tool for managing blood sugar levels, and various types of physical activity can have different effects on glucose regulation. Understanding the impact of different exercise modalities is crucial for individuals with diabetes. Here, we explore common forms of exercise and their specific effects on blood sugar control:
1. Aerobic Exercise: Aerobic exercise, often referred to as cardio exercise, involves activities that increase heart rate and breathing. Examples include walking, running, swimming, and cycling. Aerobic exercise is highly effective for improving insulin sensitivity and lowering blood sugar levels.
Mechanism: During aerobic exercise, large muscle groups are engaged, increasing the demand for energy. As a result, muscles actively take up glucose from the bloodstream for immediate use as fuel. Over time, regular aerobic exercise can lead to improved glucose uptake and better blood sugar control.
2. Strength Training: Strength training, also known as resistance training, involves activities like weightlifting, bodyweight exercises, and resistance band workouts. This form of exercise focuses on building muscle mass and can significantly impact blood sugar control.
Mechanism: Increased muscle mass enhances the body’s ability to use glucose. Muscle cells are highly insulin-sensitive, and as muscle mass increases, so does the capacity to take up glucose from the bloodstream. Stronger muscles are more efficient at maintaining blood sugar levels within a healthy range.
3. High-Intensity Interval Training (HIIT): HIIT is a form of exercise that alternates between short bursts of high-intensity activity and brief rest periods. This training method has gained popularity for its efficiency in improving fitness and blood sugar control.
Mechanism: HIIT has been shown to be particularly effective in improving insulin sensitivity. The intensity of the exercise creates a substantial demand for glucose, and the body responds by enhancing its ability to use insulin and take up glucose, even in individuals with insulin resistance.
4. Flexibility and Balance Exercises: While flexibility and balance exercises, such as yoga and tai chi, may not directly lower blood sugar levels, they offer significant benefits for overall well-being. Managing stress is essential for individuals with diabetes, as stress hormones can impact blood sugar control.
Mechanism: Stress reduction through activities like yoga and tai chi can indirectly affect blood sugar levels. High-stress levels can lead to fluctuations in blood sugar, so practicing relaxation techniques can contribute to more stable glucose regulation.
5. Everyday Physical Activity: Incorporating everyday physical activity into one’s routine is an accessible and sustainable way to contribute to better blood sugar management. Simple activities like taking the stairs instead of the elevator, gardening, or housecleaning can make a meaningful difference when performed consistently.
Mechanism: Consistent, low-intensity physical activities help maintain muscle function and promote overall health. While they may not lead to dramatic reductions in blood sugar, they contribute to an active lifestyle that supports better glucose regulation.
Duration and Frequency of Exercise for Individuals with Diabetes:
Achieving effective blood sugar control through exercise involves not only selecting appropriate types of physical activity but also considering the duration and frequency of exercise sessions. The American Diabetes Association (ADA) provides guidelines for individuals with diabetes, emphasizing the importance of regular physical activity tailored to individual needs and abilities.
1. ADA Recommendations: According to the American Diabetes Association (ADA), individuals with diabetes should aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week. This translates to about 30 minutes of exercise on most days of the week. These guidelines align with the general recommendations for maintaining good health through regular physical activity (Colberg et al., 2016).
- Moderate-Intensity Exercise: Activities like brisk walking, recreational swimming, or cycling at a moderate pace.
- Vigorous-Intensity Exercise: Activities like jogging, running, or high-intensity interval training (HIIT) that significantly raise heart rate and breathing rate.
2. Individualization of Exercise Plans: It’s essential to recognize that exercise plans should be individualized based on factors such as a person’s fitness level, age, overall health status, and specific goals. Some individuals may need to start with shorter exercise sessions and gradually progress to meet the recommended duration and intensity. For example, older adults or those with certain health conditions may need to begin with lower-intensity activities or shorter exercise bouts and gradually increase both duration and intensity over time (Balducci et al., 2015).
3. Safety Considerations: Safety is paramount when designing exercise programs for individuals with diabetes. Regular blood sugar monitoring is crucial, particularly for those using insulin or certain medications that can increase the risk of hypoglycemia (low blood sugar) during exercise. Monitoring helps individuals understand how their body responds to exercise and make necessary adjustments in terms of carbohydrate intake or medication.
- Consultation with Healthcare Providers: Before initiating or significantly changing an exercise regimen, individuals with diabetes should consult with their healthcare provider. Healthcare professionals can provide personalized recommendations and address any specific concerns or contraindications.
4. Progressive Overload: The principle of progressive overload suggests that individuals should gradually increase the intensity, duration, or frequency of exercise as their fitness level improves. This approach helps ensure that exercise remains effective in achieving and maintaining blood sugar control over time.
The Timing of Exercise and Its Impact on Blood Sugar:
The timing of exercise is a critical factor in how it affects blood sugar levels. Carefully planned exercise sessions can help individuals with diabetes achieve better glucose control. Here are some considerations regarding the timing of exercise:
1. Pre-Meal Exercise: Exercising before a meal, particularly one that is carbohydrate-rich, can be a strategic approach to managing blood sugar levels, especially for individuals with Type 2 diabetes.
- Mechanism: Pre-meal exercise helps to lower blood sugar spikes that typically occur after eating. When you engage in physical activity before a meal, your muscles use glucose from the bloodstream for energy. This can prevent a sharp increase in blood sugar levels following the meal.
- Benefits for Type 2 Diabetes: This approach can be particularly beneficial for individuals with Type 2 diabetes, as it helps improve insulin sensitivity and reduces the post-meal glucose surge (Yardley et al., 2012).
2. Post-Meal Exercise: A short bout of exercise, such as a brisk walk, after a meal can assist in glucose control.
- Mechanism: Exercise after eating encourages the muscles to take up excess glucose from the bloodstream. This helps prevent prolonged high blood sugar levels after meals and promotes more stable glucose regulation.
- Benefits for Postprandial Glucose: Post-meal exercise is particularly effective in managing postprandial (after-meal) glucose levels, which are important for overall blood sugar control (Mandira et al., 2019).
3. Regular Exercise Schedule: Establishing a consistent exercise routine, where physical activity occurs at the same time each day, can contribute to better blood sugar stability.
- Mechanism: Regular exercise, when performed consistently, helps improve overall insulin sensitivity and glucose regulation. When your body becomes accustomed to a predictable exercise schedule, it can anticipate the increased glucose demand associated with physical activity and respond more efficiently.
- Benefits for Long-Term Control: Consistency in exercise helps maintain steady blood sugar levels over time, reducing the risk of both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) episodes (Yardley et al., 2012).
Monitoring Blood Sugar During Exercise for Individuals with Diabetes:
For individuals with diabetes, monitoring blood sugar levels before, during, and after exercise is a crucial aspect of safe and effective diabetes management. Careful monitoring allows for timely adjustments to medication, carbohydrate intake, and exercise intensity to help prevent both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) during physical activity.
1. Before Exercise Monitoring: Before beginning an exercise session, it is essential to check blood sugar levels, especially if the exercise is planned close to a meal or insulin injection.
- Reasoning: Knowing your starting blood sugar level provides a baseline for determining whether it’s safe to exercise. If your blood sugar is too high or too low before starting, it may be necessary to delay exercise or make adjustments to your pre-exercise routine.
- Action Steps: If blood sugar is too high (hyperglycemia), it may be advisable to postpone exercise until it returns to a safe range. If blood sugar is too low (hypoglycemia), consuming a small carbohydrate-containing snack or drink may be necessary to prevent low blood sugar during exercise (Sigal et al., 2013).
2. During Exercise Monitoring: Continuous or periodic monitoring of blood sugar during exercise is important, particularly for activities of longer duration.
- Reasoning: During exercise, blood sugar levels can change rapidly. Monitoring allows you to detect and respond to any impending hypoglycemia or hyperglycemia. Continuous glucose monitoring (CGM) devices are valuable tools for real-time tracking of blood sugar trends during exercise.
- Action Steps: If blood sugar levels start to drop (indicating hypoglycemia), consuming a quick-acting carbohydrate source, such as glucose tablets or a sports gel, can help raise blood sugar levels to a safe range. If blood sugar rises excessively (indicating hyperglycemia), adjusting insulin doses or reducing exercise intensity may be necessary (Campbell et al., 2019).
3. After Exercise Monitoring: After completing exercise, it is advisable to check blood sugar levels to assess the impact of the activity.
- Reasoning: Exercise can lead to delayed effects on blood sugar levels. Monitoring after exercise helps determine whether blood sugar levels have stabilized, increased, or decreased as a result of physical activity.
- Action Steps: Depending on the post-exercise blood sugar levels, individuals may need to adjust their post-exercise meal or medication doses. For example, if blood sugar drops significantly after exercise, a meal or snack may be required to prevent hypoglycemia (Sigal et al., 2013).
Precautions and Safety Measures for Exercise in Individuals with Diabetes:
While exercise is a fundamental component of diabetes management, it is essential to take certain precautions and safety measures to ensure the well-being of individuals with diabetes. Here are key considerations for safe exercise:
1. Consult a Healthcare Professional:
- Rationale: Before embarking on a new exercise program, individuals with diabetes should consult with a healthcare provider, preferably one familiar with diabetes management. This is particularly important if there are underlying health issues or complications, as exercise may need to be tailored to individual needs.
- Action Steps: Healthcare professionals can provide personalized exercise recommendations, taking into account a person’s current health status, medications, and diabetes-related complications. They can also help individuals establish safe exercise goals and monitor their progress.
2. Hydration:
- Rationale: Staying adequately hydrated is crucial during exercise, as dehydration can impact blood sugar control. Dehydration can lead to elevated blood sugar levels and potentially exacerbate diabetes-related complications.
- Action Steps: Individuals should drink water before, during, and after exercise, especially in hot or humid conditions. The amount of fluid needed may vary based on factors such as exercise duration and intensity.
3. Hypoglycemia Awareness:
- Rationale: Individuals using insulin or certain diabetes medications, such as sulfonylureas or meglitinides, should be aware of the risk of hypoglycemia (low blood sugar) during or after exercise. Physical activity can increase glucose uptake by muscles, potentially leading to low blood sugar levels.
- Action Steps: It is advisable for individuals at risk of hypoglycemia to carry a source of fast-acting glucose, such as glucose tablets or a carbohydrate-rich snack, during exercise. Regular blood sugar monitoring, both before and after exercise, helps detect and address low blood sugar promptly.
4. Foot Care:
- Rationale: People with diabetes are at increased risk of foot problems due to reduced sensation and circulation. Exercise can further increase the risk of foot issues, such as blisters or ulcers.
- Action Steps: To protect their feet, individuals should wear well-fitting, moisture-wicking, and cushioned athletic shoes designed for their specific activity. Regular foot inspections are crucial, looking for any signs of injury or changes in skin condition. Any foot problems should be promptly addressed by a healthcare provider.
5. Monitoring:
- Rationale: Regular blood sugar monitoring is essential for understanding how exercise affects individual blood sugar levels. Tracking allows individuals to make informed decisions about their exercise routines and make necessary adjustments to maintain safe and stable blood sugar levels.
- Action Steps: It is recommended to monitor blood sugar levels before, during, and after exercise, as well as as-needed based on the type and duration of physical activity. Continuous glucose monitoring (CGM) devices can provide real-time data and help prevent extreme blood sugar fluctuations.
In conclusion, exercise is a cornerstone of diabetes management and plays a significant role in controlling blood sugar levels. Its benefits extend beyond glucose control, as it contributes to overall well-being and reduces the risk of diabetes-related complications. By incorporating regular exercise into their daily lives and working closely with healthcare professionals, individuals with diabetes can take control of their blood sugar levels and improve their quality of life. Always remember that the key to successful diabetes management lies in a holistic approach that includes a balanced diet, medication as needed, and an active lifestyle.
References:
- American Diabetes Association. (2016). 6. Glycemic targets: Standards of Medical Care in Diabetes—2016. Diabetes Care, 39(Supplement 1), S39-S46.
- American Diabetes Association. (2016). 9. Physical activity and diabetes. Diabetes Care, 39(Supplement 1), S47-S51.
- American Diabetes Association. (2017). Standards of Medical Care in Diabetes—2017 Abridged for Primary Care Providers. Clinical Diabetes, 35(1), 5-26.
- American Diabetes Association. (2019). 5. Lifestyle management: Standards of Medical Care in Diabetes—2019. Diabetes Care, 42(Supplement 1), S46-S60.
- American Diabetes Association. (2020). 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2020. Diabetes Care, 43(Supplement 1), S48-S65.
- American Diabetes Association. (2020). 6. Glycemic targets: Standards of Medical Care in Diabetes—2020. Diabetes Care, 43(Supplement 1), S66-S76.
- American Diabetes Association. (2021). Diagnosis and classification of diabetes mellitus. Diabetes Care, 44(Suppl 1), S15-S33. https://care.diabetesjournals.org/content/44/Supplement_1/S15
- Balducci, S., Sacchetti, M., Haxhi, J., Orlando, G., D’Errico, V., Fallucca, S., … & Pugliese, G. (2015). Physical exercise as therapy for type 2 diabetes mellitus. Diabetes/Metabolism Research and Reviews, 31(1), 13-23.
- Campbell, M. D., Walker, M., & Trenell, M. I. (2019). Large pre-and postexercise rapid-acting insulin reductions preserve glycemia and prevent early-and late-onset hypoglycemia in type 1 diabetes. Diabetes Care, 42(11), 2174-2180.
- Church, T. S., Blair, S. N., Cocreham, S., Johannsen, N., Johnson, W., Kramer, K., … & Myers, V. (2010). Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: A randomized controlled trial. JAMA, 304(20), 2253-2262.
- Colberg, S. R., Sigal, R. J., Yardley, J. E., Riddell, M. C., Dunstan, D. W., Dempsey, P. C., … & Tate, D. F. (2016). Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care, 39(11), 2065-2079.
- DeFronzo, R. A., Ferrannini, E., Groop, L., Henry, R. R., Herman, W. H., Holst, J. J., … & Zimmet, P. (2015). Type 2 diabetes mellitus. Nature Reviews Disease Primers, 1, 15019. https://www.nature.com/articles/nrdp201519
- Gibala, M. J., Little, J. P., Macdonald, M. J., & Hawley, J. A. (2012). Physiological adaptations to low‐volume, high‐intensity interval training in health and disease. The Journal of Physiology, 590(5), 1077-1084.
- Hawley, J. A., Hargreaves, M., Joyner, M. J., & Zierath, J. R. (2014). Integrative biology of exercise. Cell, 159(4), 738-749.
- Mandira, S., Dang, T. T., Mukhopadhyay, A., Khoury, D. E., Qian, J., Shantaram, M., … & Jurczak, M. J. (2019). One bout of exercise alters free-living postprandial glycemia in type 2 diabetes. Medicine and Science in Sports and Exercise, 51(6), 1236-1246.
- Perry, C. G., Lally, J., Holloway, G. P., Heigenhauser, G. J., Bonen, A., & Spriet, L. L. (2015). Repeated transient mRNA bursts precede increases in transcriptional and mitochondrial proteins during training in human skeletal muscle. The Journal of Physiology, 593(20), 4649-4666.
- Powers, A. C. (2017). Diabetes mellitus. In Harrison’s Principles of Internal Medicine (20th ed., Vol. 2, pp. 2399-2412). McGraw-Hill Education.
- Saltiel, A. R., & Olefsky, J. M. (2017). Inflammatory mechanisms linking obesity and metabolic disease. Journal of Clinical Investigation, 127(1), 1-4. https://www.jci.org/articles/view/88885
- Sigal, R. J., Kenny, G. P., Wasserman, D. H., Castaneda-Sceppa, C., & White, R. D. (2006). Physical activity/exercise and type 2 diabetes: A consensus statement from the American Diabetes Association. Diabetes Care, 29(6), 1433-1438.
- Sigal, R. J., Armstrong, M. J., Bacon, S. L., Boulé, N. G., Dasgupta, K., Kenny, G. P., … & Riddell, M. C. (2013). Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Annals of Internal Medicine, 159(4), 250-261.
- Richter, E. A., & Hargreaves, M. (2013). Exercise, GLUT4, and skeletal muscle glucose uptake. Physiological Reviews, 93(3), 993-1017.
- Rosenberg, D. E., Bull, F. C., Marshall, A. L., & Sallis, J. F. (2007). Assessing the public health potential of physical activity interventions: A case study of the Activity Multi-Optional Trial. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 27(4), 116-126.
- Wayne, P. M., & Kaptchuk, T. J. (2008). Challenges inherent to t’ai chi research: Part I—t’ai chi as a complex multicomponent intervention. The Journal of Alternative and Complementary Medicine, 14(1), 95-102.
- Weir, G. C., & Bonner-Weir, S. (2004). Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes, 53(Suppl 3), S16-S21. https://diabetes.diabetesjournals.org/content/53/suppl_3/S16
- Yardley, J. E., Kenny, G. P., Perkins, B. A., Riddell, M. C., & Balaa, N. (2012). Resistance versus aerobic exercise: Acute effects on glycemia in type 1 diabetes. Diabetes Care, 35(4), 669-675.

Former Student at Rajshahi University